Francesco P Bernardini, MD, and Brent Skippen, MD, discuss their novel technique to optimise the eyelid-cheek junction
email: francescobernardini@ icloud.com
AESTHETIC REJUVENATION OF THE periocular area is an effective intervention to address facial ageing and fatigue1. The importance of the lower eyelids, located crucially in the centre of the face, cannot be underestimated. Lower eyelid ageing is influenced by gravity and globe weight, factors responsible for the various clinical manifestations that can be sub-classified as:
- Volume changes — represented by eyelid bags and orbito-malar hollowing
- Skin changes — including skin excess and descent
- Laxity changes — manifested by eyelid margin rounding, inferolateral scleral show, lateral canthal angle medialisation, and negative canthal tilt. By widening the youthful narrow palpebral fissure, Laxity changes further contribute to the loss of perceived attractiveness2.
Traditionally, lower blepharoplasty focused mainly on addressing volume changes and skin excess in order to achieve effacement of the eyelid/cheek junction, with most authors advocating routine adjunctive ancillary procedures to prevent the downward displacement of the lower eyelid3. We believe that the added risks of these supporting procedures overcome the potential benefits and should be avoided at the time of primary blepharoplasty. We herein propose a lower blepharoplasty technique that mimics the effect of digital elevation of the eyelid skin, hence the name ‘eyelid lift’, that addresses volume, skin and laxity changes, while avoiding adjunctive supportive procedures.
Pre-operative planning
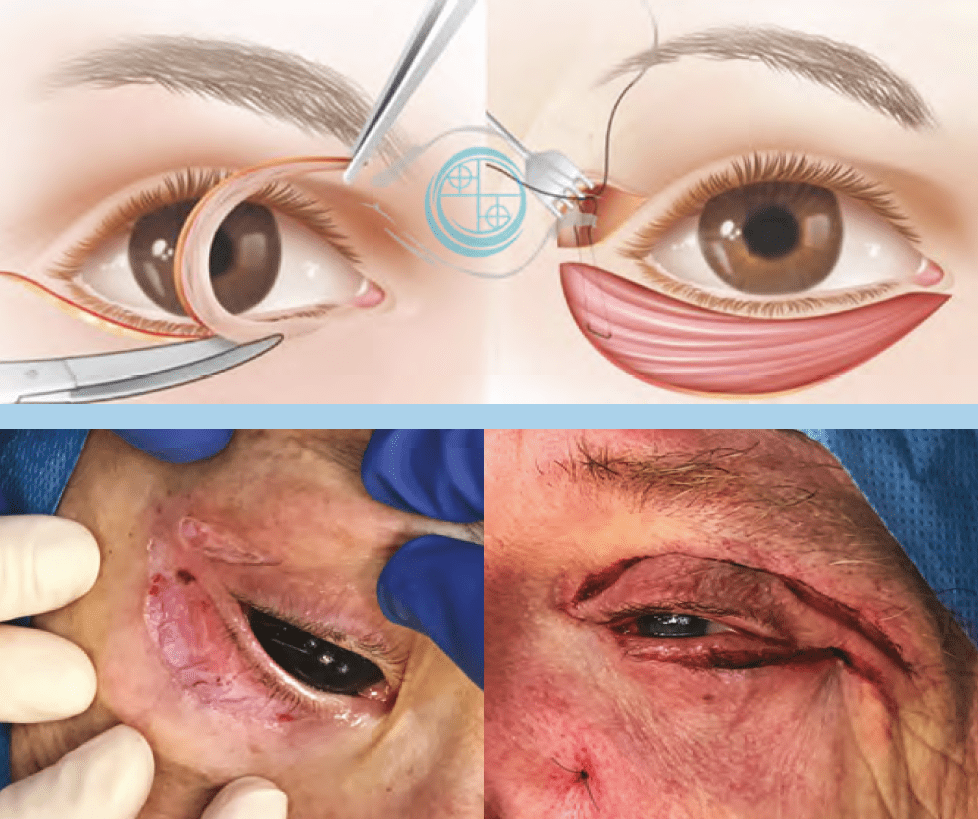
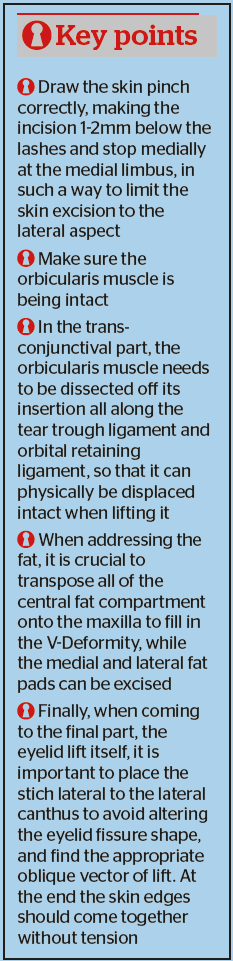
Pre-operative planning should be focused on the amount of skin excess/descent and eyelid laxity present. With the patient sitting upright, the practitioner should pinch together between two fingers the eyelid skin infero-laterally to the lateral canthus and lift vertically towards the lateral aspect of the superior orbital rim, without creating tension on the eyelid margin (Figure 1). Our approach to skin excess/laxity and eyelid laxity can be classified as follows:
- Good skin quality (no excess), typically in young patients (<35 years): use the trans-conjunctival approach exclusively
- Minimal-moderate skin descent, no skin excess
- (35–40 years): the orbicularis is exposed and
- re-draped using the orbicularis lift, without skin excision or with minimal (2–3 mm) lateral skin pinch excision
- Skin descent, skin excess and eyelid laxity, where a full ‘mini-pinch’ and lower eyelid lift is indicated
- Finally, in older patients (>65 years) with severe eyelid laxity, a canthopexy can be added to prevent post-operative complications.

A schematic approach is also applied to fat prolapse and orbito-malar hollowness based on the prevalence of the following:
- Hollowness greater than eyelid bags: complete release of orbicularis retaining ligament (ORL) and tear trough ligament (TTL) along with the ‘eyelid lift’ permitted attenuation of the demarcation caused by the ligaments
- Hollowness equal to eyelid bags: the entire centro-medial fat pad can be transposed
- Eyelid bags greater than the hollowness: medial fat pad and central fat pad separated and partially excised. In all cases the lateral fat pad was either sculpted or excised.
Pre-operative drawing
A ‘mini-pinch’ of the lower eyelid skin is marked with the patient supine with the upper marking placed just below the lashes to better hide the scar; this scar placement requires meticulous preservation of the underlying pre-tarsal orbicularis muscle. The inferior skin marking is placed in a lower eyelid skin crease, usually revealing the true amount of skin excess. Subsequently, a pinch test was performed with the patient lying supine, verifying that when pinching the lower eyelid skin, the eyelid margin maintained its position. The lateral extent of the lower marking extended to the lateral orbital rim, while medially it stopped just medial to the nasal limbus. If no upper blepharoplasty is performed, a 1 cm long incision is placed in the lateral aspect of the upper eyelid crease, maintaining a 4 mm bridge of intact skin between the upper and lower eyelid incisions.
Surgical technique
The procedure begins with transconjunctival, single-suture fat repositioning after complete release of the attachments of the tear trough ligament (TTL) medially and the orbicularis retaining ligament (ORL) laterally. The inferior septum is opened near the arcus marginalis and the fat pads dissected and carefully released. After removing the skin pinch and exposing the underlying orbicularis muscle, the ‘eyelid lift’ orbicularis suspension is performed as originally devised by one of the authors. The procedure consists of vertically elevating the un-dissected orbicularis muscle, then passing a U-shaped 6–0 polyglactin suture through the lateral part of the exposed orbicularis, to emerge at the level of the upper eyelid crease incision (Figure 2). Both needles were then passed through the periosteum overlying the lateral orbital rim supero-lateral to the lateral canthal angle and tied securely. The placement of the suture at the orbicularis level should be at the lateral third of the exposed orbicularis; if too medial, it could produce an excessively horizontal vector that might distort the eyelid margin. We recommend placing fixation at the lateral end of the superior orbital rim, in order to achieve an oblique vector. An excessively vertical placement can alter the canthal position. The amount of eyelid lift can be graded by entering the orbicularis muscle closer to the skin of the inferior incision or closer to the center of the orbicularis; the closer to the inferior skin — the stronger the lift effect.
Results
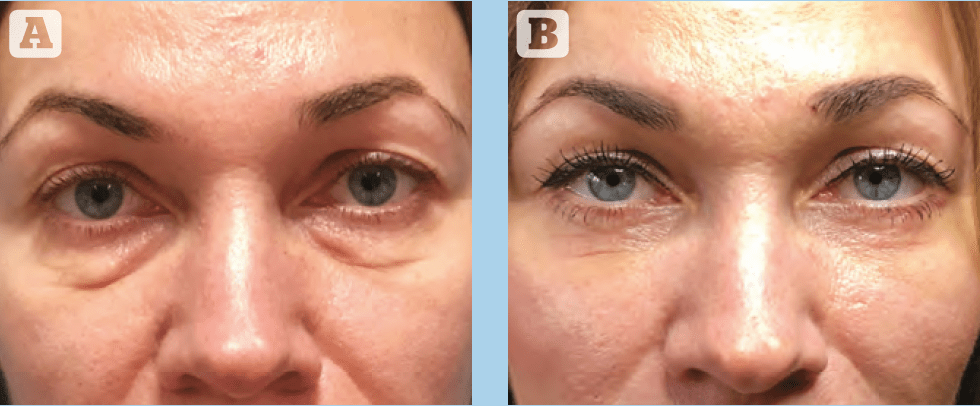
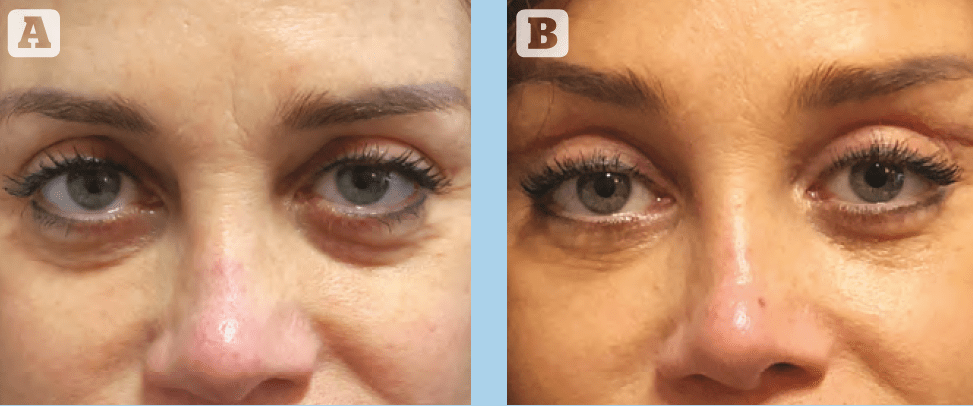
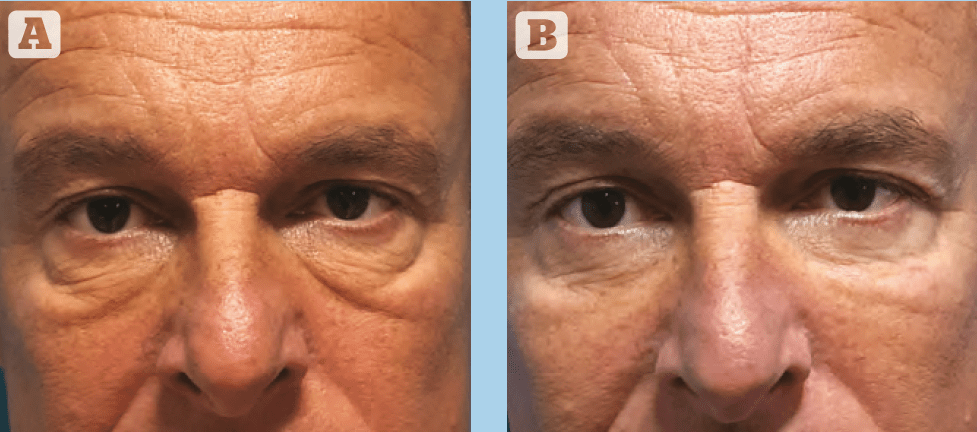
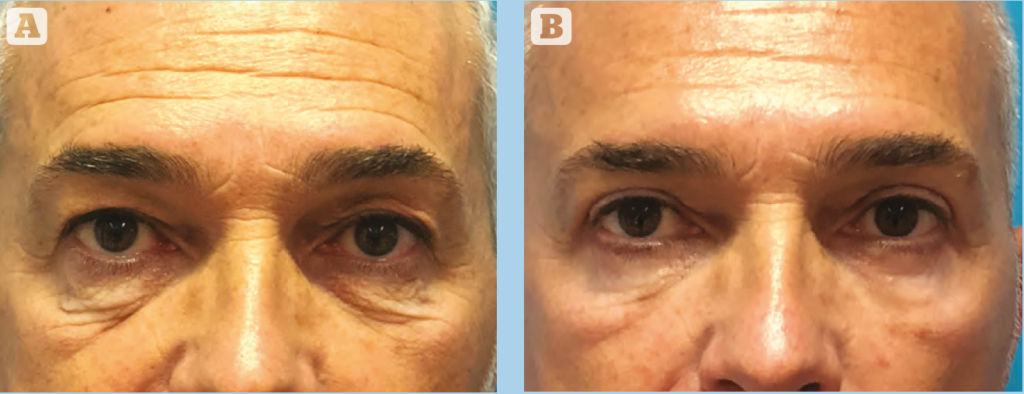
Among the 136 operated patients included in the study, 90% had subjective skin appearance improvement. Similarly, the majority of patients (96.7%) showed improvement in the tear trough contour. 75% of patients were judged to have either good (4) or excellent (5) aesthetic enhancement of this area, with the remaining 25% reporting moderate improvement (3*). No patient reported worsening effects, and no cases of cicatricial ectropion, inferior scleral show or lower eyelid retraction were observed clinically. Representative pre- and post-operative photographs are presented in Figures 3–6.
Discussion
Since Flowers’ initial report4, ‘routine canthopexy’ has become a well-established mantra among aesthetic surgeons, to the point where lower blepharoplasty can be separated into two parts: the primary aesthetic part, to correct volume and skin defects, and the second protective part, consisting of canthal tightening to provide support, as the eyelid position may be endangered by the former4.
Commonly, for patients requiring lower eyelid rejuvenation with pre-operative eyelid laxity, the literature advocated trans-palpebral mid-face lifting with aggressive skin removal followed by trans-orbital canthoplasty for even stronger eyelid support5. The role of mid-face lifting at the time of lower blepharoplasty is based on the assumption that the lower eyelid and mid-face regions are intimately interconnected structures and that drooping of the malar fat leads to the descent of the lower eyelid with rounding of the palpebral rim and scleral show. However, this approach appears to omit the latest evidence on fat compartment distribution and the strong separation between compartments provided by retaining ligaments, especially at the ORL and TTL level6,7.
We feel that these ligaments provide a functional separation between the lid and the cheek and prevent the lower eyelid following the mid-cheek ageing-induced descent. For this reason, we propose that, as the problem to be addressed is at the level of the lower eyelid, then surgeons should focus on the lower eyelid only and not recruit separate aesthetic units and do not transform a lower blepharoplasty into an unrequested mid-face lift.
The ‘eyelid lift’ technique reproduces the effects of digital elevation of the eyelid skin when pinched between two fingers and elevated laterally and above the lateral canthus — improving the volume defects, shortening the
eyelid, repositioning the lateral angle and correcting any lateral rounding of the lower eyelid margin and lateral
scleral show, without any vertical tension.
The ‘eyelid lift’ therefore represents a shift to the existing paradigm, as the orbicularis suspension component has the prominent aesthetic role, while at the same time being safe enough to not require additional steps for eyelid protection, such as canthopexy. Relative skin excess is added to the pre-existing true skin excess with the ‘eyelid lift’ procedure: the total amount of skin to be removed corresponds to the amount that can be pinched and lifted without tension on the eyelid margin. In all, the ‘eyelid lift’ permits more than adequate lower eyelid skin removal, safely and without needing to lift the cheek or provide canthal support.
Conclusions
The ‘Eyelid Lift’, consisting of a dual plane, three-step lower blepharoplasty technique, is a safe, reproducible, and effective procedure. This technique consists of simultaneous release of the retaining ligaments that contribute to the lower eyelid-cheek double convexity, volume redistribution of the two areas whilst filling the upper cheek with native eyelid fat, and elevating the eyelid in a vertical and lateral vector. The ‘Eyelid Lift’ suture is a simple maneuver of orbicularis suspension, yet it provides lifting without need for more complicated and risky mid-face procedures8.
References
- Sobanko JF, Taglienti AJ, Wilson AJ, Sarwer DB, Margolis DJ, Dai J, Percec I. Motivations for seeking minimally invasive cosmetic procedures in an academic outpatient setting. Aesthet Surg J. 2015 Nov;35(8):1014-1020.
- Rhee SC, Woo KS, Kwon B. Biometric study of eyelid shape and dimensions of different races with references to beauty. Aesthetic Plast Surg. 2012 Oct;36(5):1236-45.
- Pezeshk RA, Sieber DA, Rohrich RJ. The Six-Step Lower Blepharoplasty: Using Fractionated Fat to Enhance Blending of the Lid-Cheek Junction. Plast Reconstr Surg. 2017 Jun;139(6):1381-1383.
- Flowers GS. Canthopexy as a routine blepharoplasty component. Clin Plast Surg. 1993 Apr;20(2):351-65.
- Pascali M, Botti C, Cervelli V, Botti G. Vertical Midface Lifting with Periorbital Anchoring in the Management of Lower Eyelid Retraction: A 10-Year Clinical Retrospective Study. Plast Reconstr Surg. 2017 Jul;140(1):33-45.
- Rohrich RJ, Pessa JE. Discussion. Aging of the facial skeleton: aesthetic implications and rejuvenation strategies. Plast Reconstr Surg. 2011 Jan;127(1):384-5.
- Mendelson B, Wong CH. Commentary on: SMAS Fusion Zones Determine the Subfacial and Subcutaneous Anatomy of the Human Face: Fascial Spaces, Fat Compartments, and Models of Facial Aging. Aesthet Surg J. 2016 May;36(5):529-532.
- Bernardini FP, Devoto MH, Skippen B. The ‘‘Eyelid Lift’’ Orbicularis Suspension Technique for Lower Blepharoplasty Surgery. FPSAM 2020, 22(3):227-228