Firas Al-Niaimi evaluates the latest non-ablative fractional laser technology in two clinical cases of photodamaged skin

Facial rejuvenation treatments have become increasingly popular with the advent of various interventions with shorter downtime and faster recovery, including the non-ablative fractional laser technology. This technology is based on the fractional delivery of beams of light in columns in a wavelength that is absorbed by tissue water but below the vaporising threshold and typically in the near infrared range of 1200 and 1600 nm1. The resultant tissue interaction leads to thermal coagulation of the epidermis and dermis (depth related to wavelength and fluence used) with ultimately a wound healing process that translates into visible clinical improvements in aspects of photoaging and photodamage such as texture, fine lines, and wrinkles.
There are currently several devices in the market with wavelengths in this range with various specifications including the Candela handpiece of Frax 1550 nm with unique features such as the in-built cooling system and an adjustable scanner width2. The 1550 nm treatment has largely become one of the most sought after non-ablative fractional laser treatments.
The new Frax
1940 nm handpiece
Candela’s newest handpiece device, the Frax 1940, is a major advancement in the field of non-ablative fractional laser technology with very little matched technology available to date. The technology relies on a solid state diode emitting a 1940 nm wavelength in a scanning mode with in-built cooling (Softcool). This wavelength is unique since it lies very close to the peak of the water absorption wavelength in the non-ablative range just below the ablative threshold (1935 nm). This results in a unique avid light-tissue interaction with water with a superficially located biological interaction manifesting as coagulation and epidermal and superficial papillary dermal injury3.
Microscopic Epidermal Necrotic Debris (also known as MENDs) lead to epidermal renewal and pigment clearance, and together with the superficial nature of the injury this leads to clinically visible improvements in tone, texture, and superficial pigment clearance. There are currently very few available technologies aside from ablative lasers that have such a marked impact on the epidermis giving clinical results described by patients as: ‘glowing skin’, ‘smoother skin’, and a ‘porcelain feel’ of the treated skin.
Features of the Frax 1940 nm handpiece
The handpiece is relatively light and ergonomically friendly with an aiming beam and a disposable roller with in-built Softcool technology for comfort. The device allows for energy adjustment from 6 to 20 mj, giving an estimated depth of 200 micron. The density is adjustable between 20 and 50%, and the scanner width has the choices of 4, 6, 8, 10, and 12 mm. The latter is particularly a huge advantage as it allows for a customised treatment in smaller areas, as well as targeting with precision and maximum impact smaller lesions, such as lentigos and flat seborrheic keratoses.
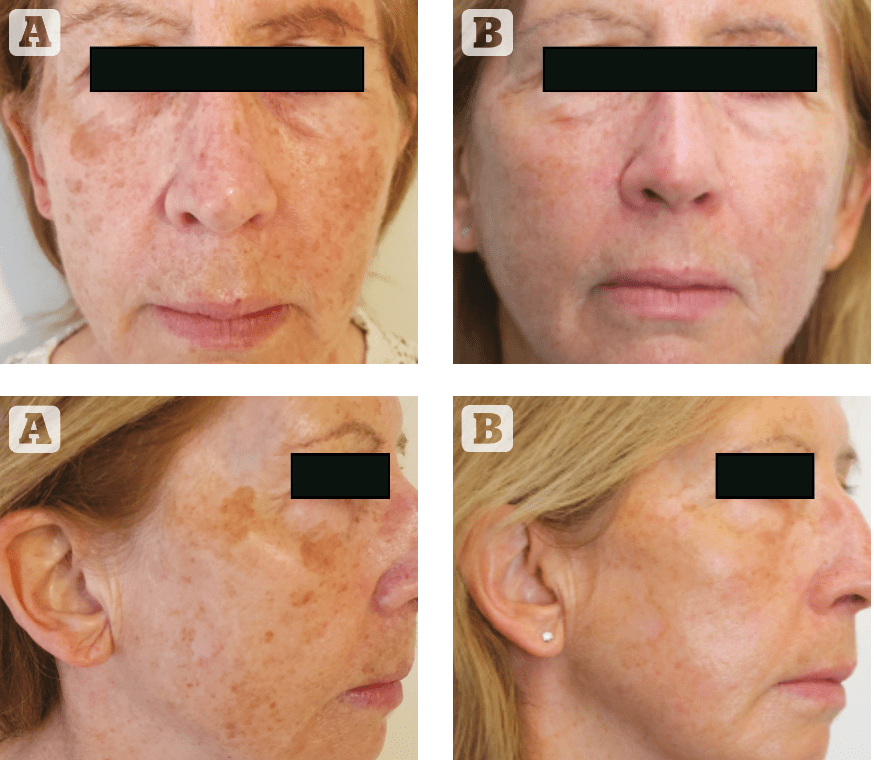
(A) Before, (B) after treatment
Case 1
A 56 year-old woman with evidence of photodamage and dull, rough facial skin was treated with the Frax 1940 handpiece, using the following parameters: Energy of 10 mj, density of 35%, scanner width of 10 mm, 4 passes over the entire face with 2 additional passes on the large individual lentigos using a 4 mm scanner width, 50% density and 7 mj fluence. The clinical endpoint is erythema and post care consisted of a light-based moisturizer regularly with strict sun protection. The downtime is around 4 to 5 days with erythema and darkening of the lentigos, and a total of 2 treatments were performed with significant improvement in pigment reduction, smoothening of the skin and the ‘glow’ described by the patient that continued for weeks post treatment.
Case 2
A 46 year-old woman with Fitzpatrick Skin Type 2 and evidence of photodamage, as well as what she described as a ‘dull and lifeless facial skin’ underwent a single treatment session using the following parameters: Fluence of 8 mj, 40% density, scanner width 12 mm, 4 passes and with softcool technology. Immediately post treatment topical vitamin C serum and non-cross-linked hyaluronic acid serum was applied to the skin. Downtime was 5 days of erythema with darkening of the superficial pigmented lesions. One month post treatment the patient reported significant improvement in the ‘feel of the skin’, texture and marked reduction in signs of photodamage. She particularly explained that her make-up simply sits much nicer on the skin and her facial skin is radiant with a glow.
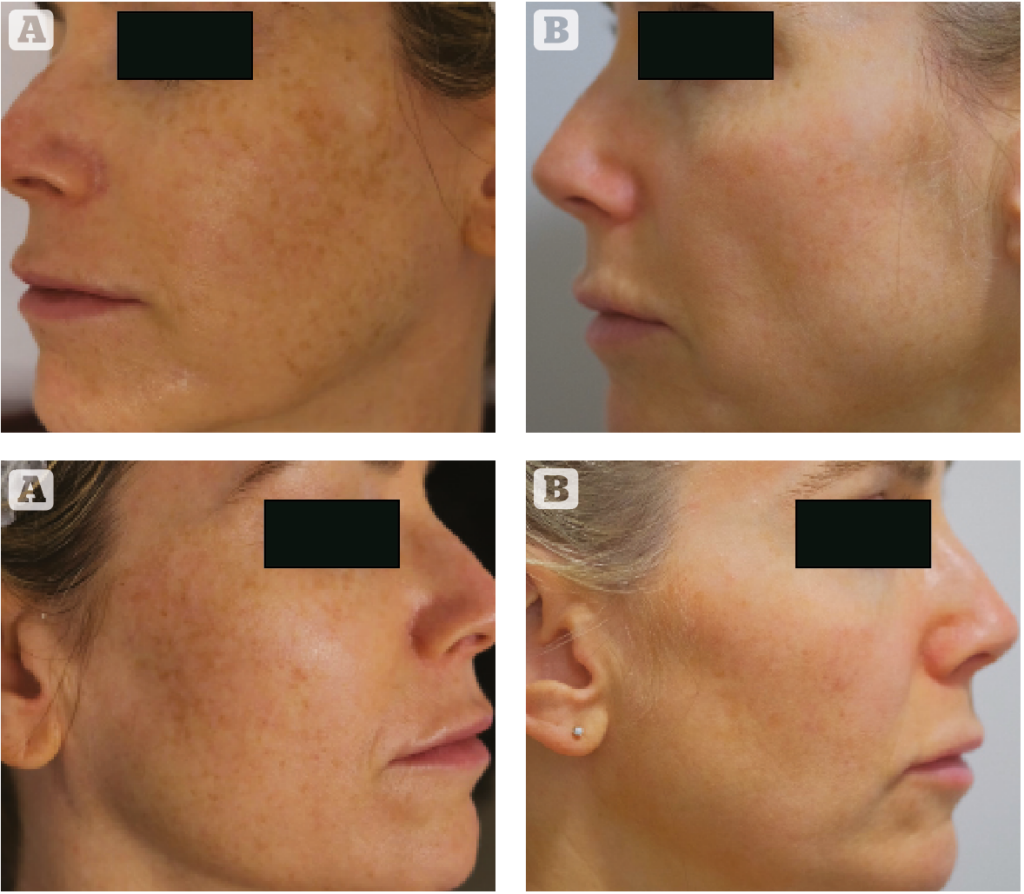
(A) Before, (B) after treatment
Find out more at: candelamedical.com
References
- Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med. 2006;38:169- 176.
- Tidwell WJ, Green C, Jensen D, Ross EV. Clinical evaluation and in-vivo analysis of the performance of a fractional infrared 1550 nm laser system for skin rejuvenation. J Cosmet Laser Ther. 2018;20:360-363.
- Miller L, Mishra V, Alsaad S, et al. Clinical evaluation of a non-ablative 1940 nm fractional laser. J Drugs Dermatol.2014;13:1324-1329.






