Natalia Markova MD, Svetlana Pervykh MD, Eliska Kubiková MD, Chuan-yuan Lin, MD, and Hsu Nai-Jen, MD discuss their novel non-surgical technique for addressing this problem area
Natalia Markova MD, Dermatovenerologist, MedicalEsthetic, Prague, Czech Republic; Svetlana Pervykh MD, Ophthalmologist, Gwangju city, Republic of Korea;
Eliska Kubiková MD, Surgeon, Anatomický ústav Univerzita Komenského v Bratislavě; Chuan-yuan Lin, MD, Head of ToBeauty Aesthetic clinic, Chief of Plastic and reconstructive division, Taipei Veteran General Hospital, Taiwan; Hsu Nai-Jen, MD, Director, Hsu Nai-Jen Dermatologic clinic, Tainan city, Taiwan
email: [email protected]
To understand and predict the results of procedures and the safety of their performance, it is necessary to understand the functional and layer-by-layer anatomy of the gluteal region4. It is bounded from above by the iliac crest, from below by the gluteal fold, from the inside by the sacrum and the coccyx (medial line — intergluteal cleft, the median ridge of the sacrum and coccyx), laterally — a line drawn from the anterior-superior iliac spine, anterior superior to the greater trochanter (trochanter NA). In the case of two gluteal folds, the lower fold is considered the border of the gluteal region. The anatomical base and the main anatomical landmarks are always bones.
In the gluteal region, there are two deep cellular spaces (deep gluteal and supratrochanteric). It is in the deep cellular space between the gluteus medius and minimus muscles that the branches of the lower gluteal vessels and nerves pass, and the fascial sheath of the sciatic nerve is located. Due to the presence of these important anatomical structures, it is undesirable to work in deep cellular gluteal spaces without using direct visualization of the above structures, which limits the work with minimally invasive technologies in this zone.
However, we are more interested in the superficial cellular space since this is the zone of impact of the studied technique. The subcutaneous tissue is well developed and penetrated by vertical fibrous cords connecting the skin and fascia. It has a honeycomb structure. To the borders of the gluteal region, the subcutaneous tissue becomes thinner and the fascial layer disappears. In women, unlike men, the layer of fatty tissue, which is located under the skin, is more developed. Fatty tissue in this area is usually elastic because it is penetrated by thin strips of dense connective tissue that go from the skin to the muscles; along the edges they are spliced with one another, forming cells that provide stability for the fatty tissue.
Materials and methods
Study population
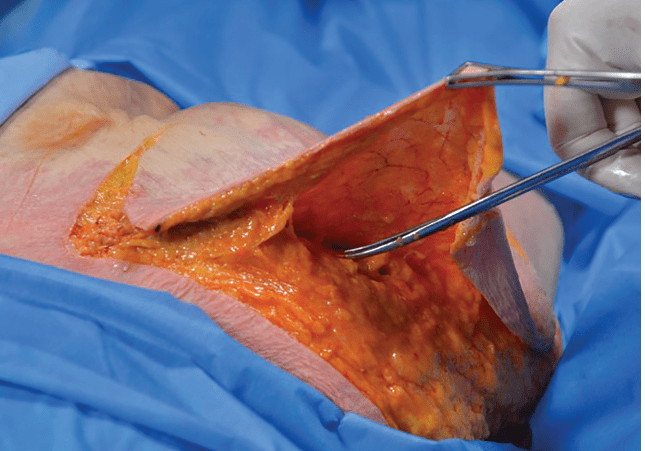
In the first part of the study, anatomical dissections were performed (8 female bodies) — age range from 54 to 83 years. The average age is 60 years. Dissections were performed at the Anatomical Institute of the Faculty of Medicine of the Comenius University in Bratislava (Slovakia) and the Faculty of Medicine of the University of Rijeka (Croatia). The research was permitted by the Ethics Committee of the Faculty of Medicine of the Comenius University in Bratislava and the Faculty of Medicine of the University of Rijeka. All rights to research and its results are reserved (Figure 1).
In the second stage, treatments were conducted on 35 women aged 35 to 53 years, with complaints of soft tissue flabbiness in the gluteal region, seeking skin strengthening and an increase in volume in the gluteal region (Beautis Malgeun Dermatology Clinic, Gwangju city, Republic of Korea) using a combined technique developed by the authors of this article.
Women without inflammatory processes and post-traumatic changes in the correction area, healthy, without permanent implants in the correction area, having no contraindications for correction, were allowed to undergo the procedure. No combined correction techniques were used in the area of correction. All patients gave their informed consent to the procedure and to the use of photo and video materials. Samples were taken from the patients for histologic examination prior to the procedure, and 5 randomly selected patients were re-sampled from the correction area (gluteal region, outer-upper quadrant) 3 months after the procedure.
This technique includes simultaneous lifting and restoration of the volume of the gluteal region, while reinforcing the gluteal region and the area of the posterior surface of the thigh, using self-fixing thread lifting and reinforcing materials as well as the administration of a collagen-stimulating polylactic acid filler.
For the lifting action5, absorbable threads with bidirectional barbs were used. As a fixing device, the Light Lift NEEDLE METHOD (manufactured by Aptos) was used: UPS 2/06; chemical composition polycaprolactone 75%, polylactic acid 25%; P (LA/CL); USP 2/0; 500 mm, 2 pcs; on needles 1.1×120 mm, 4 pcs, attached to the middle of the guide-needle7.
For their reinforcing action, absorbable threads with multidirectional barbs were used. Excellence Body Method (manufactured by Aptos), UPS 2/0; chemical composition polycaprolactone 75%, polylactic acid 25%; P (LA/CL); length 240 mm; 15 pcs; cannula 19G x 200mm; 2 pcs.
The result of the reinforcement is not immediately visible. To visualize the result, it is necessary to wait for the results of the cellular response to the implanted thread. The procedure will stimulate the production of the patient’s own collagen. This usually takes more than 1 month and intensifies by 3 months after implantation. The technique for implanting reinforcing threads is different from the technique for lifting threads. When choosing the depth of implantation, the diameter of the threads, barbs, their direction and size, as well as the purpose of implantation, are taken into account.
To stimulate collagen production, PLDA — PowerFill 1000 mg, polylactic acid 1000 mg / 24 ml was used.
Inclusion criteria
For the purposes of the procedures, it is necessary to select patients without excess weight and with an initial degree of soft tissue ptosis or in a pre-ptotic state. The degree of ptosis of the buttocks was assessed according to the classification proposed by R. Gonzalez in 2006 by the excess of soft tissues of the gluteal region, descending below the sub gluteal sulcus8.
The study included clinically healthy patients without significant chronic diseases and mental abnormalities.
All patients underwent a standard medical examination and collection of medical history to identify contraindications to thread lifting and the administration of collagen-stimulating drugs or the use of anaesthetic solutions, according to their instructions for use. The patients also signed an Informed Consent for the procedure to be performed and the use of their photographic materials for scientific purposes.
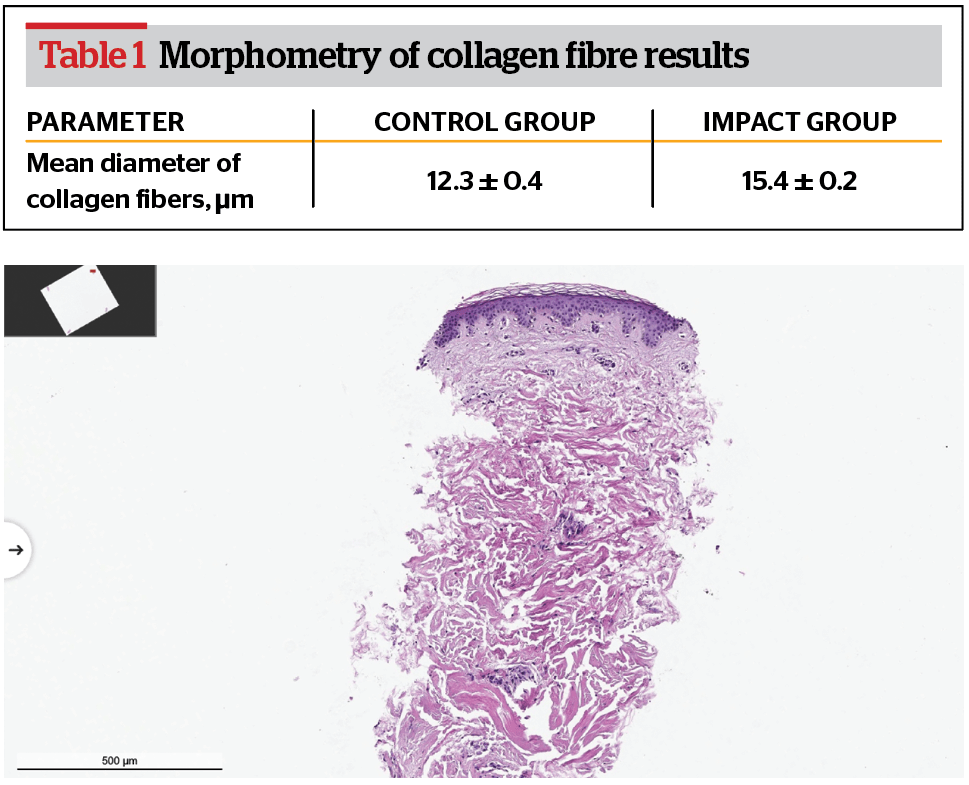
All patients underwent sampling of biological material from the area of impact by punch biopsy up to 3 mm in diameter before performing the procedures to form a control group and perform subsequent histologic examination (morphological assessment). Repeated sampling in a similar way was performed in five randomly selected patients 3 months after the procedures.

The material collected by punch biopsy for subsequent light optical examination was subjected to standard preparation:
- Fixation in 10% solution of buffered neutral formalin
- Dehydration in the alcohol series (increasing concentration)
- Exposure to xylol solution
- Embedding in paraffin with preparation blocks
- Making slices on a sledge microtome
- Staining with routine dyes
- Embedding in a stabilizing balm on slides.
The cellular/non-cellular component around the implanted materials was studied after scanning the slides using a Leica Apero AT2 scanner and random selection in sections of five random high power fields in the preparation.
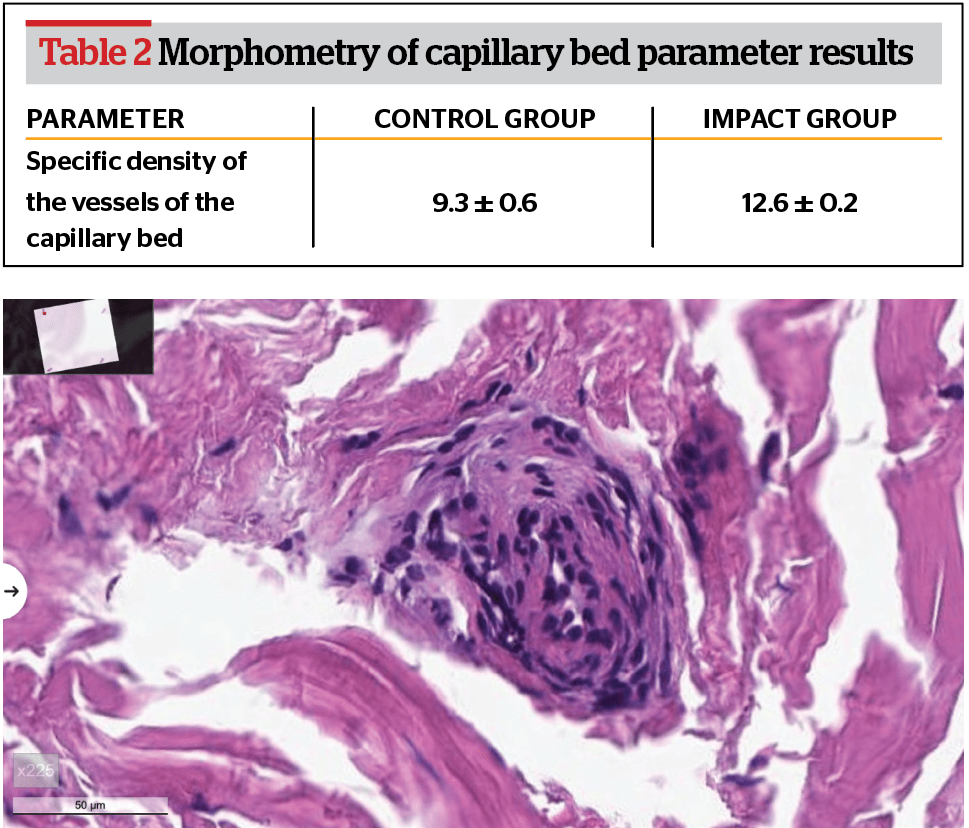
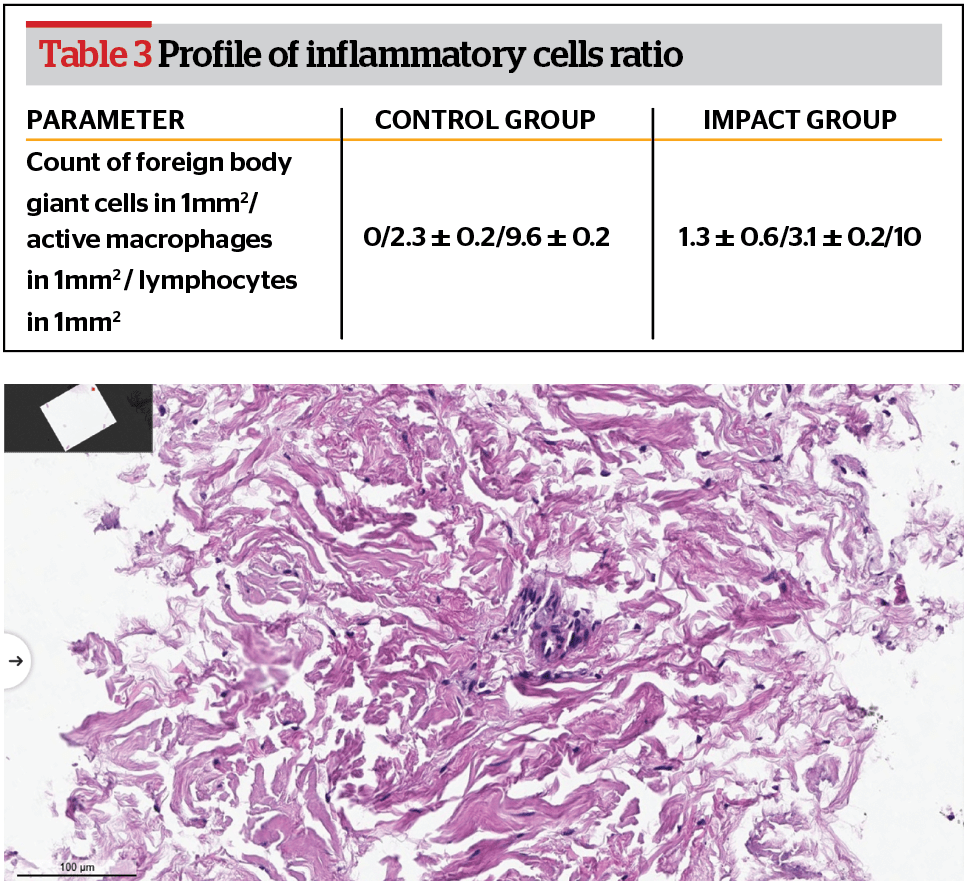
A morphometric assessment of the following parameters was performed:
- the specific area of the vessels of the capillary bed
- the mean diameter of collagen fibres
- the ratio in the profile of inflammatory cells.
Refined measurements and comparative analysis with the exposure group were made.
Procedure
To satisfy the main complaints of patients (reduced turgor and flabby skin of the gluteal region and the area of the posterior surface of the thigh, lipodystrophy and ptosis), the technique includes three successive stages:
- implantation of lifting threads
- implantation of reinforcing threads
- administration of a collagen-stimulating polylactic acid filler.
For this, the zone of each buttock is tentatively divided into four quadrants: two upper — lateral and medial, and two lower — lateral and medial. The horizontal line dividing the gluteal zone in half is the ‘sitting zone’.
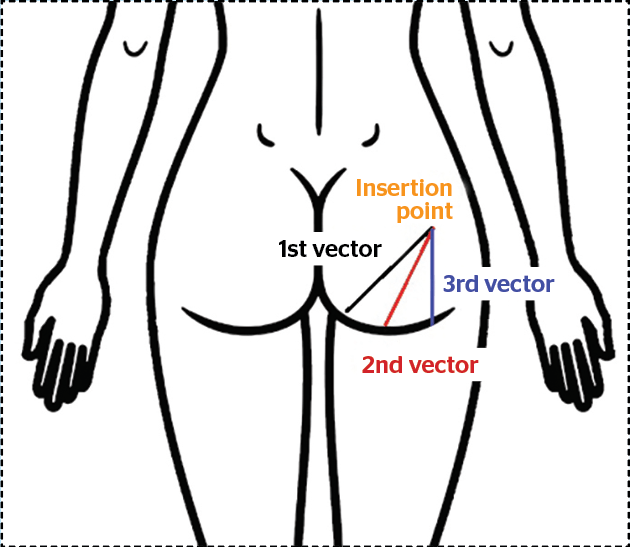
Above the ‘sitting zone’ in the upper part, according to the investigational technique, volume can be created or moved to improve the contour of the buttocks and visually lift the tissues upward. The lower lateral and medial quadrants are reinforced (Figure 2).
Before starting the procedure, preliminary photographic documentation of the impacted area is performed. Markings are made in three main stages: implantation of lifting threads, reinforcing threads, and the administration of a solution of polylactic acid.
The implantation zone is cleaned and preliminary disinfected, materials and instruments for conducting the procedure are prepared.
The polylactic acid solution is reconstituted from the dry suspension with sterile water for injection at least 30 minutes before the start of the procedure.
Anaesthesia is performed before the implants are inserted and the punch biopsy is performed. The anaesthetic solution for infiltration is chosen depending on the experience of the attending physician. First, separate injections of the anaesthetic solution are given at the cannula insertion sites. Next, infiltration anaesthesia of the implantation zone is performed. Puncture sites for cannula insertion are selected according to the length of the infiltration cannula.
After a short exposure of 5–10 minutes, before the start of the procedure, all patients underwent sampling of biological material from the area of impact by punch biopsy up to 3 mm in diameter to form a control group and perform subsequent histologic examination (morphological assessment). Repeated sampling in a similar way was performed in 5 randomly selected patients 3 months after the procedures.
Procedure stages
For the first stage, the barbed lifting thread is used to move and form volume in the upper lateral quadrant of the gluteal zone (Figure 3).
The existing volume is moved with the soft tissue lifting thread, forming it in an aesthetically more significant place (upper lateral and medial quadrants of the gluteal zone), which entails secondary improvements in tissue sagging in the lower quadrants of the gluteal zone. The gluteal region is lifted, the contours become more attractive. The result of the correction is maintained for up to 1 year.
The implantation of lifting threads is performed in a layer of deep subcutaneous fat. The injection is carried out in the upper lateral zone. We insert both needles in one puncture and then implant the thread, creating volume. By implanting the thread with the right hand, with the left hand, we simultaneously collect and maintain the volume of tissues that we want to move and fix; with a radial spreading towards the lower quadrants, pull the muscle tissues of the buttocks into the upper lateral quadrant of the gluteal zone, while simultaneously tightening and reducing the sagging of the muscle tissues in the lower lateral and medial gluteal quadrant.
For the second stage, reinforcing threads are implanted into the reticular layer of the dermis and used to reinforce the lower lateral and medial quadrants of the buttocks and the upper posterior surface of the thigh (Figure 2). The injection entry points are in the area of the upper outer quadrant. The insertion trajectory is a radial distribution in the lateral and lower sides going into the lower lateral and medial quadrants of the gluteal zone and the area of the upper posterior surface of the thigh to reinforce them.
It is recommended to use the reverse (returned) technique of one-step reinforcement and soft tissue lifting. After implantation of the first thread along the first vector, the thread is pulled with the right hand and, holding it with the left hand, the tissues are brought to the desired position, lifting and supporting them. In the same hole into which the thread has already been inserted, the thread is implanted in a reciprocating motion along the next vector. Throughout the manipulation with the thread, the tissue is held in the left hand in the desired lifted position. This creates the angle of the multidirectional vectors of the thread tension from the two halves of the implanted thread, where a lifting and reinforcing structure is held at the puncture site at the angular joint of the two halves of the thread, which, thanks to the barbs, maintains the tissues in the desired position.
Threads implanted in order to reinforce and strengthen the skin in the required zone should be implanted with as many reversals and decussations as possible since at the intersection of the implanted threads, as well as between the barbs and the thread, fibroblasts create colonies to a greater extent than merely around the implanted thread. Fibroblasts produce collagen, which creates a collagen skeleton, supporting the skin and the walls of fat cells and strengthening the skin. Hence stimulating them is very important for the reinforcement technique.
The depth of implantation of reinforcing threads differs from the depth of implantation of lifting threads. Implanting threads with the reinforcing technique, they strive to strengthen and improve the quality of the skin. Based on our histologic examinations, the best results in stimulating neocollagenesis were obtained when the thread was implanted into the reticular layer of the dermis. Stimulation of the process of neocollagenesis is the goal of the reinforcing technique of thread implantation.
For stage three, administer a collagen-stimulating drug based on a polylactic acid solution to replenish soft tissue volume.
PowerFill 1000 diluted with 24 ml water for injection was used. The total volume of the finished administered filler was 24 ml: 12 ml on each side in the area of the upper outer quadrant.
An 18 G cannula with a length of 90 mm was used to administer the drug. The drug is administered in a fan-shaped manner in different vectors and layers of subcutaneous fat. We avoid bolus injections because of the risk of overcorrection and the possible development of granulomatous adverse reactions. Such reactions are very rare but can occur due to improper dilution of the drug and non-compliance with the administration technique (overdose in a locally limited place). The drug is administered into the deep subcutaneous fat layer at the level of the hypodermis.
In addition, the required clinical result is achieved by the fact that, for the implantation of lifting and reinforcing threads for each gluteal zone, three threads of each type are used with a triple radial distribution for each of them.
Recommendations after the procedure
Antibiotic therapy with drugs, usually of penicillin or cephalosporin groups, for prophylactic purposes. The patient is advised to exclude active sports, muscle exertion in the implantation area, swimming pools, saunas, taking baths, and injury to the impacted area for 14 days.
When the drug is implanted in the gluteal region, sleeping on the abdomen is recommended for the first 4-5 days after the procedure. The patient is recommended to wear compression underwear for at least 21 days after the procedure.
Treatment of skin punctures with alcohol-based disinfectants during the first 3 days after the procedure and increased hygiene requirements are highly recommended. Do not wet the puncture sites for 3 days after the procedure.
Methods of evaluation
Clinical evaluation of the results was performed by the doctor and the patient.
The changes in the skin and subcutaneous fat in the area of impact were also assessed by comparing the histological changes in the control group (before implantation) and the comparison group, which was comprised of the biomaterial taken from patients 3 months after the intervention.
The cellular/non-cellular component around the implanted materials was studied after scanning the slides using a Leica Apero AT2 scanner and random selection in sections of 5 high power fields in the preparation.
Statistical analysis
Statistical processing was performed using the Statistica 8.0 software package. The Shapiro-Wilk test was used to assess the normal distribution of data. In the case of the normal distribution of data, the measure of the central trend was the mean (M), and the measure of dispersion was the interval between 25 and 75% of the data in the sample. The nonparametric Mann-Whitney U test was used to identify differences between groups. The parametric Student’s t-test was used to compare groups with a distribution of values that did not differ from normal. Differences were considered statistically significant at p≤0.05.
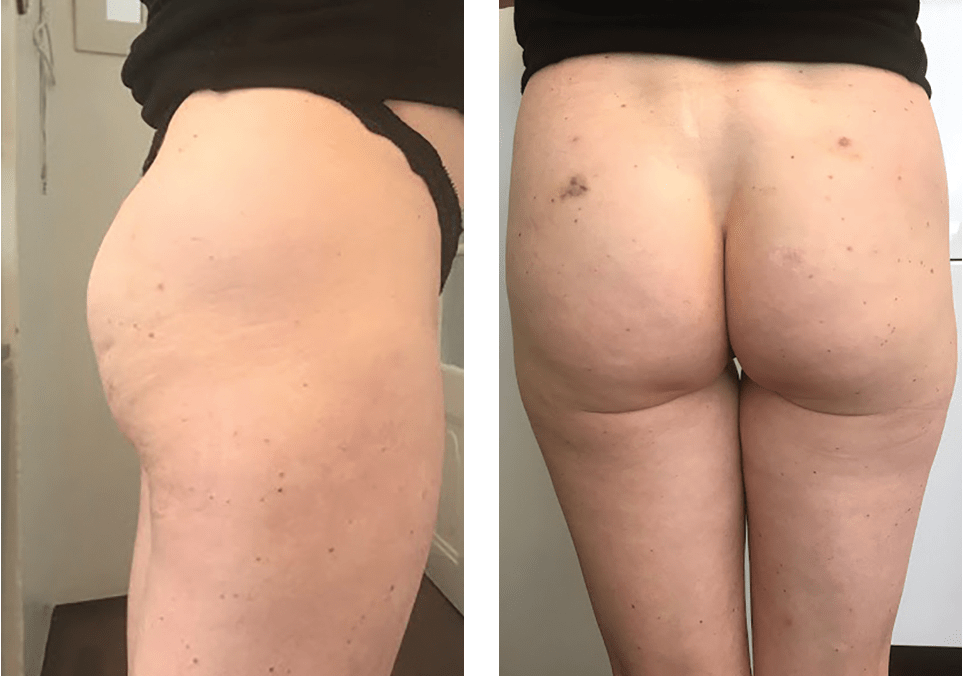
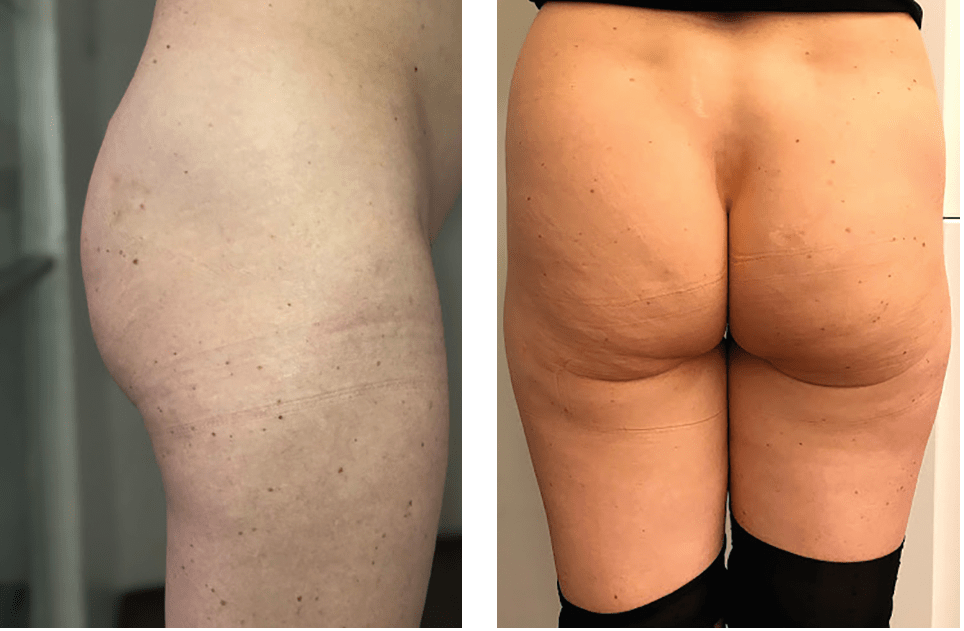
Figure 8 Photos of the female patient 21 days after the gluteal region correction procedure — lateral and front view
Results
The clinical results were assessed positively by both the doctor and the patient. The above-mentioned results were demonstrated in the creation of a visual increase in the volume of the upper gluteal quadrants, lifting the lower gluteal quadrants, reducing the degree of ptosis, and strengthening and aligning the skin surface of the buttocks and the posterior surface of the thigh, which improved the aesthetic appearance of the gluteal region and the upper third of the posterior surface of the thigh as a whole.
Results of microscopic examination of biopsy specimens
In the zone of the procedures, as a natural response to the implanted materials, both the cellular to non-cellular ratio and the quantitative indicators of the vascular density changed. The process of neoangiogenesis and neovasculogenesis is a significant indicator of the process of reorganization and tissue remodeling. There was a large presence of small capillaries in the paravasal region in the exposure group, which indicates a sufficient development of the anastomotic-capillary network.
The number of giant cells of a foreign body, active macrophages and lymphocytes were counted to assess lymphohistiocytic infiltration and calculate the ratio in the profile of inflammatory cells.

An increase in the mean diameter of the collagen fibre, as well as a change in the composition of the lymphohistiocytic series towards the predominance of cells of macrophage-monocytic representation, turned out to be significant in the exposure group. The revealed change in the parameters of the capillary bed and the change in the types of grouping of vessels require further study in order to clarify the stability and impact of these changes.
In the procedure area, as a natural response to the implanted materials, there was an increase in collagen fibre production and an increase in the mean diameter of collagen fibres. There was a change in both the cellular to non-cellular ratio and the quantitative indicators of the vascular density. The process of neoangiogenesis and neovasculogenesis was revealed, which is a significant indicator of the process of reorganization and tissue remodeling. In the exposure group, there was a large presence of small capillaries in the paravasal region, which indicates a sufficient development of the anastomotic-capillary network.
The predominance of cells of the lymphohistiocytic series was observed in the exposure group. In addition, there was a change in the composition of the lymphohistiocytic series towards the predominance of cells of macrophage-monocyte representation.
The above-mentioned data, which we obtained, confirm the clinical efficacy of the chosen approach of combining lifting and reinforcing methods with polylactic acid filler for correcting the gluteal region.
Conclusion
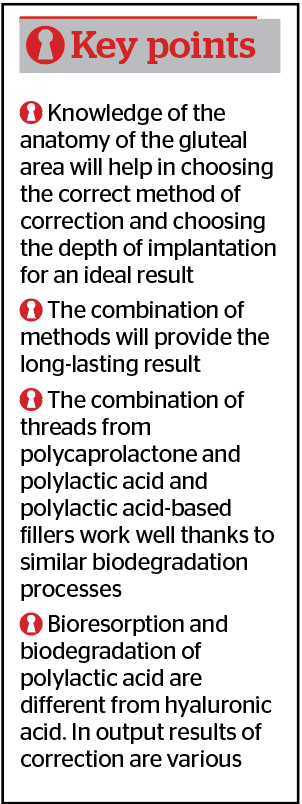
The proposed method of correcting the gluteal zone, which consists of the combined use of lifting and reinforcing threads and polylactic acid filler, satisfies the requirements of patients for skin-strengthening and an increase of gluteal volume. Anatomical studies and experiments have shown the safety of the proposed method. Histopathology reports confirmed the clinical efficacy of the method, implying the histological confirmation of an increase in collagen fibres in the area and an increase of blood supply to tissues; which, in turn, confirms an increase in the reparative capacity of soft tissues and the authors’ statement about the collagen-stimulating effect of substances that make up reinforcing absorbable threads (polycaprolactone and polylactic acid) and polylactic acid filler.
Therefore, in the proposed method of correcting the gluteal zone, the result of strengthening the skin and increasing the gluteal volume is achieved, which implies expanding the arsenal of techniques used in the field of dermatology and aesthetic medicine, and ensuring an improvement in the skin quality and non-surgical volume increase of the gluteal zone while maintaining reliability and the preservation of results..
Declaration of interest None
Figures 1–9 © Dr Markova
Tables 1–3 © Dr Markova
References
- Mills D., Rubin JP., Saltz R. Multi – Society Gluteal Fat Grafting Task Force issues safety advisory urging practitioners to reevaluate technique. ISAPS News 2018; 12: 8-9.
- Mendieta CG., Gluteal reshaping. Aesth. Surgery J., 2007; 27: 641-655.
- Sulamanidze M.A., Fournier P.F., Paikidze T.G., Sulamanidze G.M. Removal of facial soft tissue ptosis with special threads // Dermatol. Surg. — May 2002. — V. 28 (5). — P. 367–371.
- Melvin A. Shiffman, Alberto Di Giuseppe (Eds.), Body Contouring, Art, Science, and Clinical Practice / Springer-Verlag Berlin Heidelberg 2010.
- Sulamanidze M.A., Fournier P.F., Paikidze T.G., Sulamanidze G.M. Removal of facial soft tissue ptosis with special threads // Dermatol. Surg. — May 2002. — V. 28 (5). — P. 367–371.
- Sulamanidze M., Sulamanidze G., Aptos suture lifting methods: 10 years experience. Clin. Plast. Surg., 2009; 36: 281-306.
- Sulamanidze M., Sulamanidze G., Aptos suture lifting methods: 10 years experience. Clin. Plast. Surg., 2009; 36: 281-306.
- Gonzalez, Raul. “Etiology, definition, and classification of gluteal ptosis.” Aesthetic plastic surgery 30.3 (2006): 320-326.






