in the presence of dermatochalasis
Ageing and physiological contraction of the facial musculature causes wrinkles, small creases of excess skin, and skin relaxation that can take on unsightly characteristics. The removal of these imperfections can be carried out with devices using high-frequency energy (RF), which develop heat between 400°C and 600°C and rapidly vaporise intra and extracellular fluids, consequently drying the skin. To avoid this physical-chemical phenomenon, it is possible to use an electric arc with the same device, which acts without contact with the tissues, without any electrical passage between the handpiece and the skin, and without the influence of the electrical resistance of the skin. The use of the electric arc as a tool for intervention on excess skin has been reported by other authors1,2.
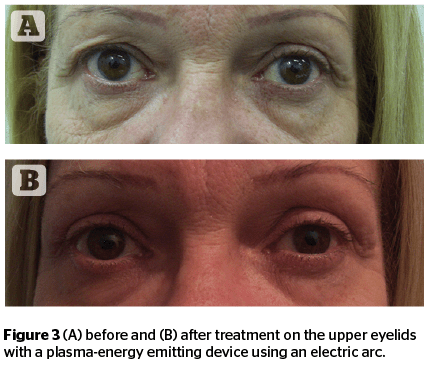
This technique is applicable to the upper eyelids in the presence of dermatochalasis and can be performed with laser devices3, RF emitting devices2, and plasma emitting devices as the authors demonstrate in this article. In order to obtain a rejuvenation of the upper eyelid, an 1800 MHZ radiofrequency device was used. Through a micro-arc, the authors obtained an effective superficial action without heating the deep tissues and retained the integrity of the dermal papillae2. To remedy the hypothetical parasitic currents or excessive tissue heating caused by RF, the authors decided later to use an instrument that develops an electric arc with plasma energy3–6.
For the rejuvenation of upper eyelids affected by dermatochalasis through the use of an electric arc with RF or plasma energy, it is necessary to analyse the mechanisms of action that contribute to the desired results. In fact, the type of rejuvenation proposed with this method is essentially the removal of small folds of the upper eyelid that are usually formed after 35 years of age3,7,8, 9–12. It is in effect an ablative and invasive surgical act, which can be performed safely on the patient with RF-emitting devices or plasma energy13.
Physio-pathological events
The authors decided to analyse the immediate effects and follow-up of a surgical approach to dermatochalasis using an electric arc. They considered the absence in the literature of a description of the physio-pathological events involved in this type of surgery on the upper eyelids. The authors also proceeded to describe, through ten years of experience and many case reports, the simple surgical procedure for the removal of blemishes from the upper eyelid, in order to standardise the methodology. This procedure consists of the elimination by micro-ablation of a portion of tissue and the physiological retraction of the remaining tissues that follows. Satisfactory use of the method is permitted in patients with mild to moderate laxity and in some cases, even severe. It is not recommended indiscriminately but in selected cases. It is not possible to compare the results with a traditional blepharoplasty5. In the surgical procedure of dermatochalasis, the epidermis of the upper eyelid is vaporised through a micro-arc8, 13, and the dermis is left partially intact. In this way, the fibroblasts and the physio-pathological mechanisms typical of tissue repair will cause the upper-eyelid to retract. The repair process follows the same pathways as wound healing only if the cutaneous appendages, sweat glands, and pilus sebaceous follicles remain intact3,9. There is, therefore, vaporisation of the superficial layers without bleeding because the epidermis is free of blood vessels. The eyelid epidermis has an average thickness of 0.2/0.5 mm that can be easily overcome during the rejuvenation of the dermatochalasis of the upper eyelids, producing aesthetic damage instead of improvement14. The removal of the eyelid creases via a micro-arc with RF or plasma emission device causes a first degree burn to the epidermis15, which will also result in the appearance of an oedema, usually lasting for 24–48 hours. The dermis would be subject to second degree burns if it is also affected by the procedure with an inflammation that can result in a functional alteration with consequent and possible damage to the anatomical structures. This type of controlled lesion triggers a healing response and epithelisation with healing and contraction of the wound8,11. The contraction takes place predominantly via the myofibroblast cells that derive from the differentiation of fibroblasts, which take on the characteristics of smooth muscle cells11 throughout the period of healing. Fibroblasts are activated by degeneration of cells of the ‘burned’ tissues and the breakup of leukocytes and macrophages. In granulation, the first cells to be initiated are the macrophages11 and the presence of scabs that appear for a few days after the treatment observed in all the patients undergoing the study confirms the scientific validity of this hypothesis.
In other similar procedures, if the treatment is repeated over two or three sessions on small portions of adjacent tissue, this would result in the tissue becoming inflamed by repeated burns. The fibroblasts that will be selected for paracrine stimulation will be fibrotic fibroblast giving rise inevitably to scar tissue14 that could seriously hinder the success of the surgical procedure or render it ineffective. Moreover, repair is a phenomenon that falters in fibrosis in the course of ageing11. It should not be forgotten that by implementing multiple sessions in adjacent portions of the same eyelid there will also be a prolonged activation of NF-KB, the main pro-inflammatory signaling pathway, which typically increases during ageing11, with inevitable lengthening of the final healing time. It will thus generate an intricate network of intercellular regulation that represents the formation of fibrosis 11, 13, 16.
For this reason, the authors never adopted a subdivisional approach when treating the eyelid, opting instead to treat the entire eyelid in one treatment session.
Reasons for the study
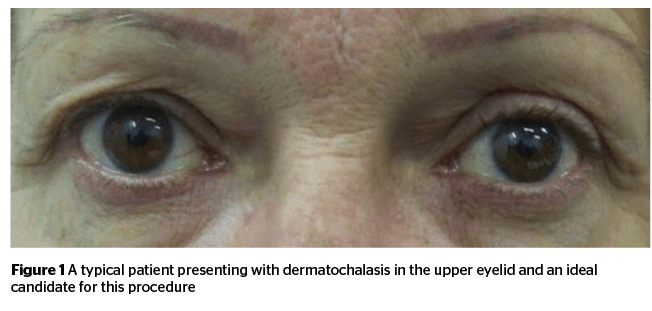
With the progress of chronological age as well as the mechanisms of ageing, many patients feel the need to intervene to create a look that addresses skin laxity and facial creases17. One such procedure looks to restore a more youthful look to the face by removing excess, lax skin from the upper eyelids without resorting to a traditional blepharoplasty. The aesthetic phenomenon that causes the physio-pathological event that requires addressing consists of the dermoepidermal relaxation of the upper eyelid until the skin folds in on itself (Figure 1).
Purpose of the study
The purpose of this study was to evaluate the results of an aesthetic improvement to the upper eyelids through an ablation with an electric arc in order to improve the look and allow for a good compromise between aesthetic need, eyelid functionality, and patient compliance15.
Materials and methods
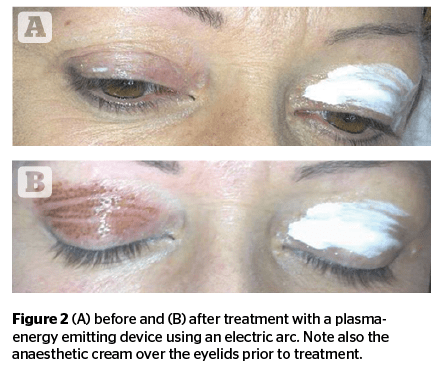
At the beginning of the study, the authors used a 1800 MHZ RF device with an electric arc. Thereafter, they began using a plasma-energy device. The aim was to selectively treat areas of eyelid tissue in order to obtain a reduction to the dermatochalasis and consequent rejuvenation of the eyelid area through selective microablation. Local anaesthesia 1 ml syringes, 30 G x 13 mm needles, lidocaine in vials was also used. The use of an anaesthetic cream used initially was soon abandoned because it was not suitable (Figure 2).
Recruitment of patients
Before starting, each subject was informed about the purpose of the study and written informed consent was obtained. No prescription drugs or cosmetic procedures were authorised for at least 2 weeks before the date set for surgical procedure. For the 132 volunteers (aged 38–81 years) between January 2008 and February 2019 that attended the clinic, the only criterion for entry into the study was the presence of dermatochalasis on the upper eyelid in addition to one or more signs of chrono or photo-ageing affecting the face, corresponding to 3–5 degrees of the photo-digital scale described by Larnier et al26.
Technique adopted
Given the need to anaesthetise the tissue, initially an anaesthetic cream was used, but after the first four surgeries, this was abandoned as it was no longer suitable. In fact, the patients on whom it had been used experienced burning sensations and/or pain more or less accentuated during and after the surgical procedure. The eyelid reddened very rapidly during surgery. Thus, the authors decided to anaesthetise the eyelid surface by injection of lidocaine through a 1 ml syringe and a 30 G sub-epidermal x 13 mm needle. In general, 0.6 ml of eyelid anaesthetic was sufficient to inhibit any sensation of burning and/or pain on all patients who underwent the study.
The authors then applied the surgical treatment with the electric arc at points 1–2 mm apart until the entire eyelid was treated, making sure that all patients received exactly the same type of procedure with the same energy, especially after the introduction of the apparatus emitting plasma-energy (Figure 2).
For 101 patients, a single treatment was sufficient to obtain the desired result. For 31 patients, a second intervention was necessary after 2 months.
Evaluation and control
Inspection visits and evaluations were made on the first day (D1, baseline) and 30 (D30) days after treatment, with a follow-up visit after 3 months. The individual signs of controlled burns, skin irritation, and the degree of correction obtained for each treatment and each area were evaluated subjectively.
All patients expressed a positive assessment of the results obtained by providing the operator with complete satisfaction, in line with the stated expectations.
Conclusions
The results obtained are certainly in agreement with the authors’ expectations of assessments on the efficacy of treatment. All the subjects treated reported to be satisfied with the general aspects of their eyelids, which appeared raised and with less accentuated folds. The burn oedema that formed within 24 hours of treatment was practically resolved in the 12 hours to follow, and any scabs healed within 4 or 6 days. These events did not prevent patients from resuming their activities. All the results after three months of follow-up have been positive.
The authors can, therefore, affirm through this study of ten years and 132 patients that the procedure of rejuvenation through a dermabrasion by means of a micro-arc with RF at 1800 MHZ or plasma-energy, which affects the dermatochalasis of the upper eyelid allows for an excellent compromise between functionality, aesthetic appearance, and expectations of the patients.
Declaration of interest No conflicts of interest or support funding
Figures 1–3 © Dr Svolacchia
References:
- Coleman , Cosmetic Surgery of the skin 1997 , Italian edition 1999 , cap. 18 , pag 277
- Sergio Camacho, timed Surgery 2000, pag 21 and 65
- Harris DM1, Fried D, Reinisch L, Bell T, Schachter D, From L, Burkart Eyelid resurfacing. J.Erratum in Lasers Surg Med 2000;26(4):415
- Harth Y, Frank I. In vivo histological evaluation of non-insulated microneedle radiofrequency applicator with novel fractionated pulse mode. Facial Plast Surg. 2014 Feb;30(1):35-9. Epub 2014 Jan 31.
- Smith JE1 Dermabrasion.. ; J Drugs Dermatol. 2013 Dec;12(12):1430-3. Lasers Surg Med. 1999;25(2):107-22.
- Scarano et A. skin lesions induced from the radiosurgical unit and voltaic arc dermoabrasion: a rabbit model. European Journal of Inflammation 9(3 (s)):89-94
- Araújo AR, Soares VPC, Silva FS, Moreira TS Radiofrequency for the treatment of skin laxity: mith or truth. An Bras Dermatol. 2015;90(5):707
- Grekin RC, Tope WD, Yarborough JM Jr, Olhoffer IH, Lee PK, Leffell DJ, Zachary CB. Electrosurgical facial resurfacing: a prospective multicenter study of efficacy and safety. Arch Dermatol. 2000 Nov;136(11):1309-16
- Parmar-Russo-Friars, 4th edition first reissue, ed. children, pp. 130, 353, 410, 453, 455, 457, Human anatomy
- Human anatomy, Balboni and others
- Giovanni Marcozzi. teaching of Surgery, third edition volume First and Second, ed. Minerva Medica, pp. 72, 74, 76
- Conf Proc IEEE Eng Med Biol Soc. 2013;2013:3761-4. doi: 10.1109/EMBC.2013.6610362. Mid-long term effect of non-ablative high radiofrequency therapy on the rabbit dermal extracellular matrix
- Carruthers et Al . Radiofrequency resurfacing: technique and clinical review. Facial Plast Surg Clin North Am. 2001 May;9(2):311-9, ix-x
- Alster T S, Jason R L. Nonablative cutaneous remodeling using radiofrequency devices.. [PubMed] Clin Dermatol. 2007;25:487–491
- Scarano et al. treatment of perioral rhytides with voltaic arc dermoabrasion; european journal of inflammation. Vol. 10, no. 1 (S2), 25-29 (2012)
- Montagner S, Costa A. Molecular basis of photoaging.. [PubMed] An Bras Dermatol. 2009;84:263– 269
- Fitzpatrick R, Geronemus R, Goldberg D, Kaminer M, Kilmer S, Ruiz-Esparza Noninvasive Radiofrequency for Periorbital Tissue Tightening. J. Multicenter Study of Lasers Surg Med. 2003;33:232– 242
- Larnier C, Ortonne JP, Venot A, et al. Evaluation of cutaneous photodamage using a photographic scale. Br J Dermatol. 1994;130:167–173. [PubMed]