The cutaneous benefits of topical retinoids are profound; their effect on remedying a myriad of skin conditions in the epidermis and dermis is unrivalled. Depending on the indication, retinoic acid or retinol may be clinically relevant. Together, these metabolites represent the current preferred evidence-based formulations for application. Their value however in achieving skin health is dependent on concentration, dosage, biodelivery mechanism, and packaging. The rise in retinol’s eminence is due to its over-the-counter accessibility, patient compliance, anti-ageing properties, and melanocyte stabilisation. Initially, topical retinoids incite reactions, a favourable sign of product efficacy. Should one hope to procure the innumerous benefits of vitamin A, it is essential for these to occur. The management of anticipated reactions is a key concept for physicians to grasp, if patient compliance and outcome is to be maximised.
Imagine all of the key cells within the skin: keratinocytes, melanocytes, fibroblasts, and angioblasts. Think of their individual roles, and the intricate interactions occurring daily between such structures, and their respective layers. Now throw diseased states into the pot, and for spice, pickle that with both intrinsic and extrinsic ageing. The physiological scope of cellular function and dysfunction, now becomes mesmerising yet extensive. Is it possible for a single topical agent to target all of the cutaneous cells, maximise and synchronise their functions, while simultaneously reversing the evil that is disease and ageing? Absolutely, and that’s precisely why vitamin A gets the superhero mark of distinction.
The beginning
Most superheroes have a backstory, which explains how they acquired their abilities, and vitamin A’s began over 3500 years ago in ancient Egypt. The recommended cure for endemic night blindness was ‘roasted ox liver, pressed, applied (to the eye)’, and this was deemed particularly effective1. Egyptian medicine was partly empirical, partly magical. It was believed that this method transferred the remedy to the afflicted eye, by way of the ox’s strength. Interestingly, the patient’s sight improved, but this contradicts what we know today in modern medicine: vitamin A is only delivered to the retina systemically. Hence, night blindness caused by a loss of rhodopsin in the retina, would not yield to topical therapy despite juice of ox liver being rich in vitamin A. An amusing sidelight to this mystical treatment that scholars later discovered, is that the practitioners fed the remaining organs to the patient1. But, this was never considered part of the night blindness therapy.
Extraordinary abilities
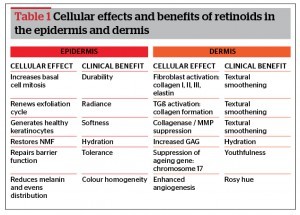
Topical retinoids have profound benefits on the epidermis and deeper layers of the skin (Table 1)2–22. Tissue effects are mediated by their interaction with specific cellular and nuclear receptors3. The cytoplasmic unit includes the cellular retinoic acid binding protein (CRABP) types I and II, and the cellular retinol binding protein (CRBP). Retinoic acid receptors (RAR) and retinoid X receptors (RXR) form the nuclear binding sites. The former is specific for trans-retinoic acid, while the latter for 9-cis retinoic acid. Through their direct effect on stimulating gene expression, retinoids are able to regulate cellular functions, and provide potent therapeutic benefit for a legion of skin conditions3–6. Notably, even after their application has ceased, amelioration can last for up to 4 months9.
Within the epidermis, retinoids activate basal cell mitosis, and healthy keratinocytes are generated6. By thickening the epidermal layer, they fortify the protective capacity of the skin. The keratinocyte cycle is also enhanced, and the exfoliative process restored to 6 weeks, providing a characteristic ethereal ‘glow’5. Stratum corneum is compacted, while keratin composition becomes more gelatinous, lending to a softer, smoother outward appearance5,20–22. Additionally, the water, lipid, and protein balance is repaired, thus restoring barrier function and reversing sensitivity. Melanin formation is further decreased, and existing pigment digested and distributed evenly to surrounding keratinocytes2,8.
Regarding the dermis, retinoids have been shown to stimulate fibroblast activity, and alter the core matrix components5. Neocollagenesis (type I, II, and III) occurs through increases in transforming growth factor beta (TGβ) and procollagen, while collagenase activity is simultaneously suppressed21,23. A surge in elastin deposition can also be witnessed histologically, leading to a reduction in surface lines and wrinkles. Glycosaminoglycan (GAG) and natural moisturising factor (NMF) production are further upregulated, so that innate hydration is re-established. Angiogenesis also increases, maximising the delivery of nutrients, and the removal of waste materials9. This enhancement in cutaneous circulation is likely responsible for the improved wound healing observed with retinoids24.
Vitamin A topical therapy, however, does not incite permanent cutaneous change. Discontinuation or significant truncation of use will cause regression of clinical gains24.
The cast of characters
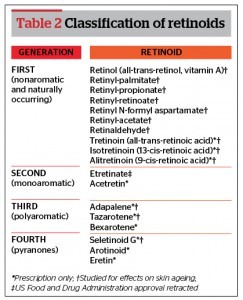
Retinoids are a family of compounds composed of vitamin A, its derivatives, and synthetic molecules acting through the same pathway. They can be classified using their chemical makeup (presence of aromatic groups), generation, composition (natural or synthetic), and availability (prescription or over-the-counter [OTC])24. Table 2 displays a comprehensive list of retinoids using a range of existing classifications24.
Retinoids are naturally existing elements acquired through diet. Vitamin A cannot be synthetised by the body, and so this must be supplemented in the form of retinyl esters from animal sources (e.g. liver, eggs), and beta-carotene from plants (e.g. carrots, spinach)3. Once ingested, they are absorbed through the small intestine and converted into retinol. Retinol is then delivered by the bloodstream to target cells, where it is either stored as a retinol ester (palmitate, propionate, and acetate) or oxidised to intracellular retinoic acid through a theorised two-step process, with retinaldehyde serving as the intermediary3. Retinoic acid represents 50% of the active cellular form, with its metabolites (4-hydroxy-retinoic acid), stereoisomers 9-cis-retinoic acid (alitretinoin), and 13-cis-retinoic acid (isotretinoin) making up the difference24.
Ingestion of vitamin A, however, does not correlate with dermatologic merit. Irrespective of the volume consumed, vitamin A is preferentially distributed to the muscles, brain, bones, and liver. A nominal amount is delivered to the skin through the oral route. Topical application of the vitamin is therefore essential in order to reap the cutaneous benefits.
Vitamin A exists in four topical forms: retinoic acid, retinol, retinaldehyde, and retinyl esters. The latter three must undergo cutaneous conversion to a more active metabolite (retinoic acid), whereas the former is applied in the pharmacologically functional state3. With use spanning over half a century, retinoic acid remains the most studied derivative; yet it still necessitates a prescription. An increasing demand by patients for cost-effective, non-invasive methods to improve the appearance of skin had led to the other vitamin A topicals gaining favour. Clients are turning away from controlled medications and procedures, and are instead considering OTC treatments such as cosmeceuticals, with less downtime. This may be owing to a lack of insurance coverage for prescription products to treat ageing, the need to pay for physician visits to obtain a controlled medication, and/or failure to discern ‘fact from fiction’ related to unsubstantiated claims by OTC skincare products23.
The parallel rise in interest for non-prescription retinoids within the scientific community and skincare industry is palpable. However, their clinical value was for many years limited, due to obstacles in product formulation. Using retinol as an example, Kligman was a forerunner in identifying and advocating its use, but creating an acceptable agent was seemingly impossible. It was irritating in therapeutic doses, easily deactivated, malodorous, and delivery to deeper cutaneous structures where it was most needed remained inadequate25. Current retinol formulations using novel chemical engineering and biodelivery systems are able to circumvent such hurdles to garner the benefits.
An overview of topical retinoids and their current applicability in clinical practice is provided below.
Retinoic acid
Retinoic acid is essential when treating diseased states, or when the practitioner chooses to deliver a ‘strong punch’ for skin rejuvenation. It may also be employed to successfully prepare the skin before a procedure (e.g. chemical peel, dermabrasion)24. This results in significantly faster re-epithelialization with more rapid healing (2 days earlier), reduced post-inflammatory hyperpigmentation and milia formation. Evidence does not however support its use in pre-treating skin before a CO2 ablative laser, but it is perhaps useful for fractionated and erbium resurfacing24.
When retinoic acid is topically applied, it is the end form, the acid, that exists both extra- and intracellularly. The extracellular component generates reactions (erythema, scaling, xerosis, and pruritus) similar to any other acid when applied to the skin, because of the exposed carboxyl group in the polar end of the retinoid3,23–25. These anticipated reactions, typically lasting 6 weeks, are requisite in order for the skin to build tolerance and repair itself16.
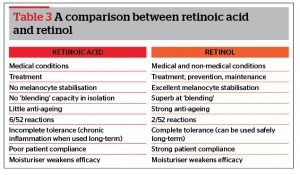
As only 30% of cutaneous cells are active during any given period, retinoic acid should be employed for three keratinocyte maturation cycles (18 weeks), in order to successfully capture all structures. After such time, retinoic acid can be discontinued, for it has delivered its maximal therapeutic benefit, which is primarily epidermal (dermal remodelling is not seen until 52 weeks). Beyond this 18 week treatment interval, retinoic acid’s irritating properties instead prevail, and this may result in chronic inflammation (Table 3)16. Furthermore, long-term studies of its effect on skin are limited to 6 years and prove inconclusive24. Evidence does however suggest that continued vitamin A therapy is preferable for dermal refashioning, but via a less irritating topical form16,24. Alternatively, a lower concentration of retinoic acid can be employed, and less frequently applied3, 16, 24.
Retinol
Considering all retinoids, retinol remains the most commonly encountered and fruitful OTC variant. This is owing to successful advances in stabilising the molecule and cost effectiveness. Its anti-ageing potential was realised in 1995, when Kang et al. first presented the ability of retinol to induce epidermal thickening and enhance the expression of cellular retinoic acid-binding protein II (CRABP II) and cellular retinol-binding protein (CRBP) messenger ribonucleic acid (mRNAs), and proteins24. Moreover, this occurred with little irritation as the carboxyl group of retinoic acid is replaced by a hydroxyl group in retinol. By 1996, Duell had formally demonstrated that retinol could be as effective as retinoic acid in producing ‘retinoid mediated histological changes’ but with greater patient compliance3. Further studies revealed that it provides a more effective delivery of a retinoidal effect compared with retinoic acid. A comparison of 0.25% retinol with retinoic acid 0.025% showed increased cutaneous penetration of the former over the latter with substantially less irritation26.
The indications for retinol use are far greater in contrast to retinoic acid21. It can be employed for both medical and non-medical conditions, prevention, maintenance, anti-ageing, and melanocyte stabilisation16. When applied to the skin, retinol is the natural form of vitamin A, which the cells are accustomed to being presented with. Once this is taken up intracellularly, it is then converted to the active pharmacologic state, retinoic acid27,28. Reactions are therefore reduced, because the irritating acid component is restricted to within the cell. These typically last for only 2 weeks, and patient compliance is therefore improved16,29,30. Retinol can be safely applied long term because, unlike retinoic acid, cells are able to build tolerance to it without inciting chronic inflammation (Table 3)16,21,31.
Retinaldehyde
Retinaldehyde is the intermediate compound formed when retinol is oxidised to retinoic acid3. Its appeal over topical retinol is owing to a postulatory faster bioconversion to retinoic acid via a one step process. However, this potential pathway is controversial. Some authorities instead debate that retinaldehyde converts primarily to retinol by the enzyme retinol dehydrogenase32. Irrespective, under varying microenvironments (e.g. hydrolysis, molecular cleavage, oxidation-reduction) other pathways can take effect over the theoretical primary and yet, retinaldehyde must undergo in vivo conversion to a more active metabolite24. Clinical studies support the aforementioned views, as topical retinaldehyde’s superiority over retinol is not scientifically qualified. The linear dose-response is lost with retinoid concentrations in excess of 0.25% retinol or 0.5% retinaldehyde26. Also, its efficacy in converting to the active form (retinoic acid) appears weaker (0.8%) in comparison to retinol (2%)23.
Conversely, some studies have revealed that retinaldehyde is propitious to retinoic acid. In two large randomised controlled trials for treating photodamaged skin, retinaldehyde and retinoic acid had similar improvements on profilometric scores. However, retinaldehyde was better tolerated throughout the studies24. This is because its metabolism occurs only by keratinocytes at a pertinent stage of differentiation, leading to a more controlled delivery of retinoic acid3. Moreover, intrinsic to the retinaldehyde compound is an antimicrobial and comedolytic effect, but this has yet to be proven in an in vivo model24. While the limited evidence in support of retinaldehyde is promising, statistically significant, histologic and long-term studies still need to be performed3,23,24.
Outside of a few literature references, retinaldehyde is not commonly employed, and OTC availability is lean33. This is because of multiple impediments that exist when attempting to formulate an effective topical34. The molecular size of reinaldehyde is considerably large, and its epidermal penetration poor. When encapsulated in a liposomal delivery system, it enters the dermis via the hair follicle but with significant financial cost34. Additionally, like other retinoids, retinaldehyde is an unstable molecule that easily degrades. This chemical engineering hurdle has been overcome with retinol formulations but not as yet with retinaldehyde. Overall, retinaldehyde is an appealing vitamin A derivative in concept, but its role in current practice remains limited and controversial.
Retinyl esters and derivatives
Retinyl esters (e.g. retinyl-palmitate, retinyl-propionate, retinyl-acetate) serve a primary role in cellular storage of vitamin A, with retinyl palmitate being the predominant form33. For clinical activity, they too must undergo conversion to retinoic acid. Development was prompted by the side-effects of retinoic acid therapy, and instability of retinol33. However, no subjective or objective evidence exists in support of their use over vehicle controls23,24. A study by Green over 48 weeks showed that topical retinyl propionate cream (0.15%) did not demonstrate any statistically significant improvement over placebo in any of the evaluated histopathological or clinical symptoms of photoageing3.
Special powers
Retinoic acid’s potency is indisputable and it remains the ‘protagonist’ in evidence-based skincare24. While there are a host of OTC retinoids, retinol is unquestionably the pre-eminent choice and will remain the focus of this article3,16,23,24. Its capacity for anti-ageing and melanocyte stabilisation is particularly appealing and is further juxtaposed here16.
Anti-ageing
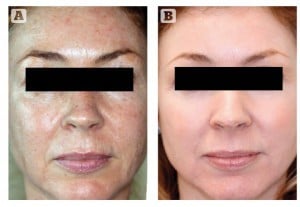
Figure 1 Photoageing, solar elastosis, and ephilides. Patient shown (A) before and (B) after treatment for 12 weeks with 0.1% retinoic acid (ZO Complex A™ and ZO Melamix™)
Retinoidal smoothening and wrinkle effacement results from epidermal hyperplasia, compaction of the stratum corneum, thickening of the granular layer, and increased epidermal and dermal glycosaminoglycan (GAG) deposition24. Retinoids further increase collagen content in the upper papillary dermis, and inhibit their degradation through collagenase and matrix metalloproteinase (MMP) suppression2,5,8. Specifically, type I procollagen biosynthesis is increased and type I, III, and VI (dermal-epidermal anchoring fibrils) collagen production is upregulated by up to 80%24. This retinoidal reorganisation of dermal collagen into new woven bundles is thought to indirectly stimulate elastic tissue normalisation24. Furthermore, the ageing gene on chromosome 17 is blocked11,16. Together, these appreciable alterations lead to a reduction in photodamage, wrinkles, and elastosis (Figure 1).
With advancing age and UV exposure, vascularity also dwindles. Skin colour mirrors this, and changes from a rosy pink hue to a dull gray complexion. By 30 years of age, there is a 25% reduction in cutaneous circulation, and at 50, there is a 60% decline16. The only topical agents shown to improve angiogenesis and vascularity are retinoids14,18.
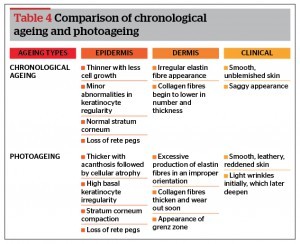
Although primarily and extensively studied in correcting photoaged skin, retinoids also illicit benefit upon chronologically aged skin (Table 4). While only one vehicle-controlled clinical study has been undertaken, the magnitude of morphological change suggests that retinoidal effect may be greater for intrinsically aged than for extrinsically aged skin3,24.
Retinoic acid was initially heralded as the champion of managing ageing, but this concept has recently been revisited. Retinoic acid yields a significant amount of reactions. These hostile conditions seemingly generate a cellular distaste for the product. As such, only a small amount is taken up intracellularly, and so the cumulative benefit of retinoic acid is limited16. Moreover, patient cessation rate is high due to reaction intolerance, and so benefits are finite.
Comparatively, when retinol is applied, it is in the preferred topical state. Reactions are far fewer compared with retinoic acid, and a greater amount of product is allowed to enter cells17,21. The nuclear benefits are therefore superior, and this includes anti-ageing26. Specifically, retinol decreases the appearance of wrinkles through the increased production of GAGs (which retain substantial amounts of water), and collagen30. Patient compliance also dramatically improves, affording long-term gains. This is especially relevant in sensitive skin clients as outlined by Kligman, which in one German study represents as much as 82% of females and 63% of males24. Given that the vitamin’s benefits are cumulative, retinol is therefore the more auspicious anti-ageing treatment option.
Equally notable is retinol’s activity in the dermis. Ageing in this cutaneous layer is pronounced, yet it remains the hardest to target with topical agents. Only 2% of retinoic acid reaches the dermis, irrespective of the volume used. But through scientific advances in targeted delivery systems, retinol can be biovectored to forcefully penetrate deeper dermal layers by up to 20%, so as to capitalise on the anti-ageing capacity of vitamin A23.
Clinical trials show both statistically significant histologic and subjective improvements with retinol in as little as 7 days24. Its use in elderly patients (mean age of 87) has also been evaluated, with dramatic benefits seen especially in relation to dermal stimulation23.
Melanocyte blending and stabilisation
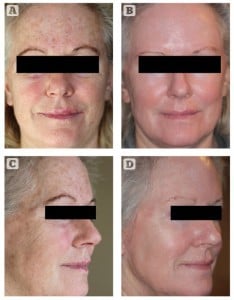
Figure 2 Photoageing, solar elastosis, and ephilides. Patient shown (A, C) before and (B, D) after treatment for 12 weeks with 0.65% retinol (ZO Retamax™)
Retinoic acid is thought to reduce hyperpigmentation by enhancing epidermal cell turnover. This decreases contact time between keratinocytes and melanocytes, promoting a faster shedding of pigment23. Comparatively, retinol also promotes epidermopoiesis, but has an additional ‘blending’ capacity; it pushes existing pigment into neighbouring keratinocytes, thereby improving skin tone16. Retinol may be employed to successfully treat ephelides, post-inflammatory hyperpigmentation, photodamage, and non-specific skin discolouration. A 2005 controlled clinical trial evaluated the efficacy of retinol (0.3%) and hydroquinone (4%) against retinoic acid (0.05%) in the treatment of photoageing. Interestingly, the retinol–hydroquinone combination diminished the collective signs of photodamage more effectively than retinoic acid3,24. This included dyspigmentation, fine wrinkles, and tactile roughness over 16 weeks of treatment.
However, when managing conditions of pigmentation, and patients prone to these disorders, it is relatively easy to tidy up the discolouration. The difficulty arises afterwards, when attempting to control the chronic wild cells that made the mess, and prevent it from recurring. Retinol has outstanding capabilities at stabilising melanocytes16. It essentially muzzles these cells, making them less responsive to negative stimuli. Typically, diseases of pigmentation return easily once treatment has ceased, in response to triggers such as heat, inflammation, UV radiation, and hormonal fluctuations. But with retinol’s ability to render the melanocyte less reactive, such flares can be circumvented. Retinol use is therefore a crucial tool following treatment of diseases such as melasma with hydroquinone16. It can be safely used long-term (unlike hydroquinone) for maintenance, to control the melanocytes, and avoid pigment recurrence20. Of note, retinoic acid is not capable of stabilising melanocytes and its long-term role is inconclusive24.
Kryptonite
Moisturisers weaken the potency of retinoids. Pharmaceutical companies frequently drench their vitamin A products with excessive, biologically irrelevant emollients to reduce the anticipated reactions36. This limits product efficacy and results, in exchange for patient comfort. Steroids are a similar culprit added to lessen retinoid reactions. These are equally detrimental, especially when used long term (side-effects include telangiectasia, skin atrophy, and striae), and they nullify any potential benefit of the retinoid.
Retinoids are unstable compounds, and so correct packaging is critical to maintain bioavailability. They are deactivated on exposure to oxygen, light, heat, humidity, lipid-peroxidation, water, and bacteria24,35,36. It is therefore imperative that the retinoid be encased in an airtight, UV protective system. A pump mechanism of delivery is also preferable. Such packaging will maintain product efficacy, while dispensing accurate volumes according to the surface area being treated.
Strength
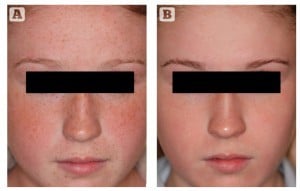
Figure 3 Ephilides, and familial pseudocutis laxa. Patient shown (A) before and (B) after treatment for 6 weeks with 1% retinol (ZO Brightenex™)
Superheroes are widely recognised for their worth and contribution to society. As such, companies capitalise on them through clothing and other marketing materials. But if a civilian dons a superhero’s costume, it will not empower them with the same formidable strength. Likewise, simply because a retinoid is advertised on a product, it does not imply efficacy19.
Using retinol as an example, scientifically researched beneficial concentrations range from 0.4% to 1%24,33. The average OTC products contain 0.08% or less24,33. Furthermore, they are packaged in open jars or tubes, both of which will allow rapid deactivation of the already inadequate concentration of retinol. Moreover, the retinol delivery mechanism is just as important as concentration and packaging17. Uncontaminated 10% retinol may be theoretically placed on the skin, but unless this is formulated to penetrate the epidermis, nothing will transpire. It is analogous to attempting to fit an earthmover into a single car garage. However, once the retinol is able to penetrate the stratum corneum, it can be biovectored to deliver its load upon different structures, making it a truly dynamic force.
The value of retinoic acid is also influenced by the formulation18. Gels and lotions cause excessive irritation, and primarily beget epidermal improvement. They are appropriate when treating diseases of seborrhea such as acne3. Cream vehicles should alternatively be used for anti-ageing purposes. These provide greater dermal benefit, and the emollient base drives patient compliance3,12. More recently, liposome and nanoparticle carriers have been studied, mostly in animal models3,24. Nanoparticle delivery systems have shown the most promise, by not only decreasing local side-effects but also significantly increasing drug efficacy. The concentration of retinoic acid is also key; higher levels correlate with deeper, more potent effects3,24. Formulations of 0.05%–0.1% yield both epidermal and dermal benefits, while levels < 0.025% have mainly epidermal effect.
It is worth clarifying that retinol and retinoic acid concentrations are not directly equatable. Retinol’s potency is approximately 5% that of retinoic acid’s, and so a higher concentration is required when formulating16.
The weapons
To overcome their foes, superheroes are equipped with an arsenal of weapons. Similarly, clinicians have ZO® Skin Health to tackle cutaneous nemeses. This prescription grade skincare line offers a comprehensive portfolio of efficacious vitamin A products. These are all replete with antioxidants, barrier repair ingredients and natural anti-inflammatories. Kim and colleagues have demonstrated that such concomitant application is valuable at counteracting the retinoids irritant effects, and optimising patient adherence3. The ZO armamentarium is as follows:
ZO Retamax™
Retamax™ employs the use of a microemulsion retinol delivery system. This allows for rapid penetration through the epidermis, and carpet bombs the dermis. The 0.65% retinol is therefore primarily delivered to the fibroblast cells, causing collagen upregulation (Figure 2). This unique chemical engineering makes the product exceptional at surface texture remodulation (e.g. scars, patulous follicles, phymatous changes). Serecin protein is further added to enhance collagen I production through biomimicry, and to bathe the dermal matrix in hyaluronic acid so that it does not become dry and brittle.
ZO Brightenex™
Brightenex™ uses oleosome technology, which is a vehicle that resembles the skin’s phospholipid bilayer. Retinol 1% is impregnated into these spheres, which easily penetrate the skin due to their small circumference. The osmotic pressure change in the epidermis causes the oleosomes to release their load on the keratinocytes and melanocytes. Brightenex™ therefore capitalises on retinol’s potential at improving discolouration and stabilising melanocytes, by surgically striking these cells. Interestingly, Brightenex™ is the only product currently available on the market that successfully combines retinol with vitamin C. The latter enhances pigment clearance and melanocyte stability, while also reducing reactive oxygen species that trigger the inflammatory cascade and ignite melanogenesis. Brightenex™ can be used to both treat existing discolouration, and prevent the onset of new pigmentation through melanocyte stabilisation (Figure 3).
ZO Radical Night Repair™
Radical Night Repair™ employs Oleosome technology, to cleverly deliver a colossal dose of 1% retinol. The vehicle is engineered to simultaneously target the epidermis and dermis, thereby maximising the retinol’s holistic and anti‑ageing potential. Upon application, the product is slowly drizzled through the skin, allowing for a controlled delivery of the high concentration retinol. This limits irritation and drives patient compliance. Humectants, barrier repair agents, antioxidants, and a unique anti-inflammatory complex further offer a multimodal approach at limiting irritation, and maximising therapeutic outcome.
Retinoic acid
Both 0.05% and 0.1% retinoic acid in cream vehicle are available through ZO. The Kligman style of high strength treatment favours the latter. This is because greater retinoic acid concentrations induce faster improvement in skin appearance (clinically and histologically), and more ‘rapid retinization’. Patient compliance and satisfaction is therefore strengthened. In a drug with delayed gratification and local side-effects, this method is preferential. The 0.05% can be used in dry/sensitive skin, or for pulsed maintenance in recalcitrant disease.
Reactions
Initially, retinoids dehydrate the outer surface of the stratum corneum while keeping the desmosomes intact. This leads to rapid, coarse shedding of an attached group of cells13,14,20,21. The so called ‘retinoid reaction’ is thought to be initiated by the release of pro-inflammatory cytokines (Figure 4)16,25. Depending on the vitamin A topical selected, anticipated reactions can either last 2 weeks (retinol), or 6 weeks (retinoic acid)21. As the treated skin begins to accommodate product application, the associated signs and symptoms subside.
It is important to remember that reactions are a favourable sign of product efficacy25. They signify the repair of damaged keratinocytes, increased basal cell mitosis, and the restoration of hydration. Should one hope to procure the innumerous benefits of vitamin A, a short controlled period of initial reactions is necessary. This is especially true when addressing disease, which represents a state of chronic inflammation. The only agreed upon method of reversing chronic inflammation, is the induction of a short, pulsed period of acute inflammation, that is, reactions16.
However, reactions don’t equate to suffering, they occur along a spectrum. Physicians must educate patients on how to control them, so that there exists a moderate degree of reactions, but the patient is neither too comfortable nor too uncomfortable. If the reactions are overly pronounced, the patient may skip the retinoid for 1–2 days16. This will allow the skin to heal, and gradually build tolerance. Moreover, vitamin A should never be applied to damp skin as this can provoke excessive reactions3,24.
Like other superheroes, vitamin A enlists the help of a supporting cast in difficult times. This is in the form of a nourishing agent, which soothes the skin during reactions. Traditional inert moisturisers should be avoided during this time, as they weaken the potency of retinoids, and lengthen the overall reaction period16. Instead, a comprehensive calming agent (e.g. ZO Restoracalm™) may be enlisted, rich in humectants, relevant lipid fractions, anti-inflammatories, antioxidants, and barrier nourishment25. Restoracalm™ also contains ingredients to repair and protect DNA, growth factors to support cellular function, and hydrolysed serecin to upregulate hyaluronic acid production.
Another corollary to consider with topical retinoid therapy is photosensitivity24. Much like the retinoid reaction, photosensitisation typically arises at the start of therapy, and gradually resolves. Patients should be advised to avoid excessive sun exposure, and include a comprehensive, broad spectrum, sunscreen (e.g. ZO SunSmart™) in their daily regime24.
Systemic side-effects have not been reported in the three decades of retinoid application3. Moreover, Lattarino and colleagues found that topical tretinoin had no detectable effect on endogenous plasma levels of retinoic acid or its metabolites3. This is mainly because of the limited transdermal uptake of these agents. Although teratogenicity from topical use has not been described, pregnant women should be instructed to discontinue treatment owing to a lack of concrete evidence3. Notably, one retrospective control case study of 215 mothers exposed to retinoic acid in the first trimester had lower rates of birth defects than the control group24.
Conclusion
The therapeutic, evidenced-based benefits of vitamin A are vast, these are well documented and indisputable. Depending on the indication, retinoic acid or retinol may be clinically relevant, but their value in achieving skin health is dependent on concentration, delivery mechanism, and packaging. Practitioners must be urged to look beyond the smoke and mirrors of pharmaceutical mismarketing when selecting their vitamin A product. Furthermore, the management of anticipated reactions is a key concept for physicians to understand, if patient compliance and outcome is to be maximised.
If you want to know what lies behind the mask of a 3500 year old superhero, its flawless skin: smooth, soft, tight, disease free, hydrated, full, firm, and tolerant to the many evils of the environment. KAPOW !