More Than a Difficult Cosmetic Patient
Chris Kowalczyk, Gregory Bartos, Amelia Damse, Andrei Gherghina, Sabrina Fabi, Steven Dayan, and Shino Bay Aguilera examine an often overlooked body dysmorphia condition presenting in aesthetic patients

Kowalcyzk C. DO, SPGY-2 Clinical Research Fellow, Oceans Dermatology and Mohs Surgery, Boynton Beach, FL, USA; Bartos G. DO, PGY-3 Dermatology Residency Training Program, LCH/LECOM, South Miami, FL, USA; Damse A. DO, Oceans Dermatology and Mohs Surgery, Boynton Beach, FL, USA; Gherghina A. DO, SOceans Dermatology and Mohs Surgery, Boynton Beach, FL, USA; Fabi, SG, MD, FAAD, FAACS, Department of Dermatology, University of California, San Diego, California; Dayan SH. MD, Departments of Otolaryngology and Dermatology, University of Illinois and Private Practice (SDMD), Chicago, Illinois; Aguilera SB. DO FAAD, Shino Bay Cosmetic Dermatology and Laser Institute, Fort Lauderdale, FL, USA;
email: [email protected]

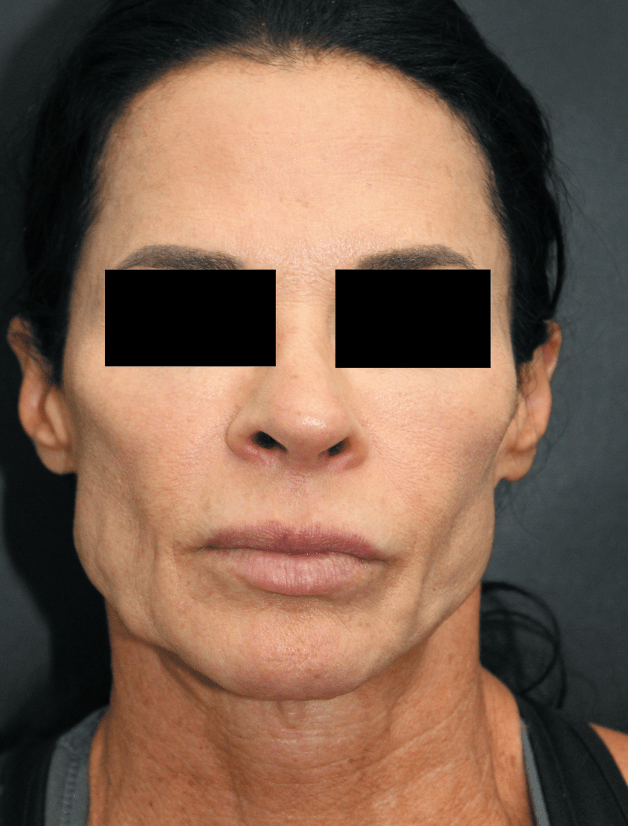
A stereotypical vigorexic female patient does everything right
but takes it too far
The internet’s social media landscape and its increasingly accessible body of information interact such that patients are now aware of an array of surgical and non-surgical cosmetic interventions. This growing awareness, knowledge, and accessibility has led to a rise in the prevalence of cosmetic procedures over the last two decades1. However, this abundance of information hosts an unregulated barrage of filtered and unfiltered depictions, which can create unrealistic cosmetic pursuits due to drifted perceptions2 and body dysmorphic disorder (BDD). As a medical community, we advocate for lifestyles that promote wellness, but now we have a population that is inundated by health gurus, targeted ads, influencers, and even our colleagues across multiple platforms. One phenomenon rearing its head as an emerging challenge in this ever-shifting landscape is vigorexia, the confluence of these concepts coming to bear.
Vigorexia, a portmanteau of vigor and –orexia, is a term for describing the unhealthy, Sisyphean appetite for health and youthfulness. Specifically, this is not referring to or attempting to malign good habits, responsible cosmetic application, or anxious individuals; instead, this term embodies a portrait of a previously undescribed population that is anecdotally growing. This group is often composed of voracious, educated, type-A personalities that eventually develop their knowledge of healthy living into addictive and vicious behavioral cycles. In the aggressive pursuit of these once adaptive routines, this vigorexic population go on to conversely suffer from premature signs of ageing.
In order to understand why vigorexic habits result in a backlash for the patient, one must first acknowledge that certain patterns of subcutaneous fat are a primary quality of a youthful face and body. Regarding a normal gynecoid habitus, breast, thigh, and buttock fat can be signs of fertility and youth. The natural and youthful contours of a young face are the reflections of both bony anatomy and buoyant fat pads. Natural ageing and gravity lead to decreases and displacement of this type of lipid deposition; hence, the aim of subtle, tasteful, professional installation of injectable cosmetics is a mimicry of the once abundant subcutaneous facial fat. In pursuit of a slim trimmed body, the over-dieting, over-exercising, and over-anxiety burgeon into extreme restrictions and deleterious routines, resulting in global fat loss, which may lead to prematurely aged appearances in the face and other healthy fat deposits.
Why vigorexia is a problem
Given that speciality diets have created a $71 billion industry3, it is unsurprising that so many patients are trying one in order to maintain a balanced weight. It is also unsurprising that so many will also undergo rapid weight loss, losing track of where the healthy becomes unhealthy. Names like paleo, keto, and intermittent fasting, which boast real advantages and some medical repute, become marketed as ‘lifestyles.’ In a vigorexic patient who becomes obsessed with calorie restrictions and low-fat intake, their decreasing body mass index (BMI) and global fat loss diminish natural contours at the aforementioned points of their silhouette. This excessive pursuit of fat loss precipitates a lean-to-gaunt appearance in the face, requiring surgical and non-surgical cosmetic interventions to restore the former beauty.
In addition to global fat loss, excessive exercise and calorie restrictions may lend themselves to endocrine abnormalities. Secondary amenorrhea, not uncommon in women with rapid weight loss, can also lead to an appearance of premature ageing in those who obsessively exercise or diet. Secondary amenorrhea predominantly affects young, unmarried females, with over 50% of all participants citing cosmetic reasons for dieting4. This change in the ovulatory cycle leads to decreased oestrogen, a constituent driver of healthy skin. Demonstrably, hormone replacement therapy in post-menopausal women increases and restores epidermal hydration, skin elasticity, and skin thickness5.
Vigorexia poses a novel challenge in those who perfectly understand the role of cosmetics in volume replacement, but are unaware of how their boosted metabolism, specifically living in upregulated, catabolic lipolysis, affects fat stores. In a self-defeating cycle, vigorexic patients will replace their self-induced fat deficit with cosmetic injectables and continue with intense exercise regimens, up-shifting their metabolic demands and thereby losing the benefits of fillers more rapidly. Unavoidably, these scenarios result in an unhappy patient—one who may grow accusatory about product quality, selection, dilution and the physicians’ abilities. Even more alarming, it may present an opportunity for predatory practitioners to retain a patient who will always demand more product despite yielding little medical benefit.
Currently, no literature directly comments on how a constant state of catabolism leads to a shorter half-life for injectable hyaluronic acid (HA) fillers and neuromodulators. Purdom et al.6 (2021) demonstrated that subjects who were exercising to the point of non-functional overreach (NFOR) versus normal training had a 34.5% decrease in muscular HA. In short, NFOR is a state in which muscles are unable to perform fully due to overexertion in serial workouts. Although this study focused on HA and its role in muscle recovery, this may hint at a physiologic basis for the observed decrease in efficacy of HA fillers that has been noted in our vigorexic patients. This proposed decrease in efficacy may be responsible for more frequent cosmetic visits before routine timelines would suggest.
Another possible hormone participating in the vigorexic’s ageing process is cortisol. Although body dysmorphia, a central facet in this population, is not classified as an anxiety disorder, we know these patients to be much more anxious at baseline. As in any change to homeostasis, but with constant, global stress especially, cortisol excretion rises. There is a known relationship between these elements: mental stress leads to increases in cortisol, which leads to telomere shortening7. These patients, hyperfocused on their wellness, are ironically causing premature cellular ageing.
The solutions for approaching vigorexia are not expeditious. The first step is physician awareness, recognizing these patients who on paper may seem to be thriving but whose exercise and dieting behaviours are excessive and potentially harmful. Intervention begins with a slow-moving, individualised approach in which a practitioner will explain, and likely need to re-explain, how the cycles of over-dieting and over-exercising intersect with cosmetic injectables. After educating and counselling the patient regarding their behaviour, expectations on injectables need to be established. Expectations should include the practitioner’s reasoning in product selection, product placement, and estimated duration of action. It is also incumbent upon such a practitioner to recommend alternatives to excessive exercise regimens, such as yoga, and to educate the patient on available injectables that may be better suited for their desired outcome and duration. Finally, despite education and tempering expectations, the word ‘no’ may be a requisite tool in the approach to the vigorexic patient.
Intervention
This excessive appetite for health and youthfulness in the vigorexic patient is noted within multiple cosmetic practices. Although appealing because they are primed to be returning frequently, focus should be placed on awareness of the constellation of appearances, outward behaviours, and inner thought patterns for this affected patient population so that intervention can begin. As a collective, practitioners are unlikely to change the messaging sprawled across the internet for constantly updated health obsessions, but on the individual level, regular opportunities will present where we can educate and intervene in this population to ensure the best cosmetic and physiological outcomes.
Declaration of interest All authors contributed to this manuscript. All authors of this manuscript have no conflicts of interest to disclose.
References
- American Society of Plastic Surgeons. ASPS National Clearinghouse of Plastic Surgery Procedural Statistics. 2020 plastic surgery statistics report. https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf
- Sola CA, Fabi SG. Perception drift. Dermatol Surg [Internet]. 2019 [cited 2022 Jan 22];45(12):1747–8. Available from: https://pubmed.ncbi.nlm.nih.gov/30985338/
- Lau A. How dieting became a $71 billion industry, from Atkins and Paleo to Noom. 2021.
- Nakamura Y, Yoshimura Y, Oda T, Kamei K, Iizuka R. Amenorrhea due to weight loss. Nihon Sanka Fujinka Gakkai Zasshi [Internet]. 1984 [cited 2022 Jan 22];36(5):727–35. Available from: https://pubmed.ncbi.nlm.nih.gov/6376664/
- Stevenson S, Thornton J. Effect of estrogens on skin aging and the potential role of SERMs. Clin Interv Aging [Internet]. 2007 [cited 2022 Jan 22];2(3):283–97. Available from: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2685269/
- Purdom TM, Wayland A, Nicoll JX, Ludwar B, Fry A, Shanle E, et al. Intramuscular hyaluronic acid expression following repetitive power training induced nonfunctional overreaching. Appl Physiol Nutr Metab [Internet]. 2021 [cited 2022 Jan 22];46(12):1563–6. Available from: https://pubmed.ncbi.nlm.nih.gov/34437821/
- Steptoe A, Hamer M, Lin J, Blackburn EH, Erusalimsky JD. The longitudinal relationship between cortisol responses to mental stress and leukocyte telomere attrition. J Clin Endocrinol Metab [Internet]. 2017 [cited 2022 Jan 24];102(3):962–9. Available from: https://pubmed.ncbi.nlm.nih.gov/27967317/








