Tinchia Hsu, MD, and Yuchin Tsai, MD, discuss an easy and approachable method for perioral volume restoration and rejuvenation
Ageing encompasses volume deteriorations that affect bone and tissues1–5. In perioral ageing, resorption of underlying bone and dentition1, together with loss of soft tissue volume, can manifest as reduced upper lip volume, tissue elasticity, thickness, and contour, alongside vertical rhytids, lip ptosis, vermilion border eversion, and skin photoaging or altered texture1,3,6–8. The entire perioral area encompasses the orbicularis oris, levator labii superioris, levator labii alaeque nasi, depressor angular oris, depressor labii inferioris, and risorius9. However, the ‘J’ shape that is characteristic of younger lips is achieved by the orbicularis oris, while the ‘I’ shape associated with ageing occurs due to upper lip elongation and concavity10. Consequently, perioral rejuvenation procedures have increased in recent years11 and traditionally involve autologous fat transfers, filler injections, and perioral laser resurfacing12 to modify perioral volume change, enhance perioral definition, and improve rhytids and marionette lines12.
Dermal fillers, customarily used in facial volumisation or to relieve static rhytids and folds and restore volume loss13–17, have been shown to change muscle movement in specific structural deficiencies. Known as myomodulation, this phenomenon describes how dermal fillers, especially hyaluronic acid (HA) fillers, alter the activity of facial mimetic or sphincter muscles they are strategically placed within or beside13,18, and could potentially be used to deliberately change facial musculature19,20. HA filler-based myomodulation was also postulated13 to affect muscle function following placement in specific injection planes and tissue depths, while muscle function was hypothesised to have been increased by submuscular fillers but reduced by supramuscular and intramuscular fillers. This was supported21 by observations that sub-mentalis fillers markedly reduced mentalis hyperactivity, suggesting that placement depth was an important consideration in myomodulation. However, we believe that the intramuscular fillers are responsible for this activity since the mentalis originates from the mandible. Whether myomodulation facilitates or obstructs muscle action 13,22–24 remains unclear, and myomodulation with HA fillers is still a novel strategy as published data on treatment outcomes is limited25.
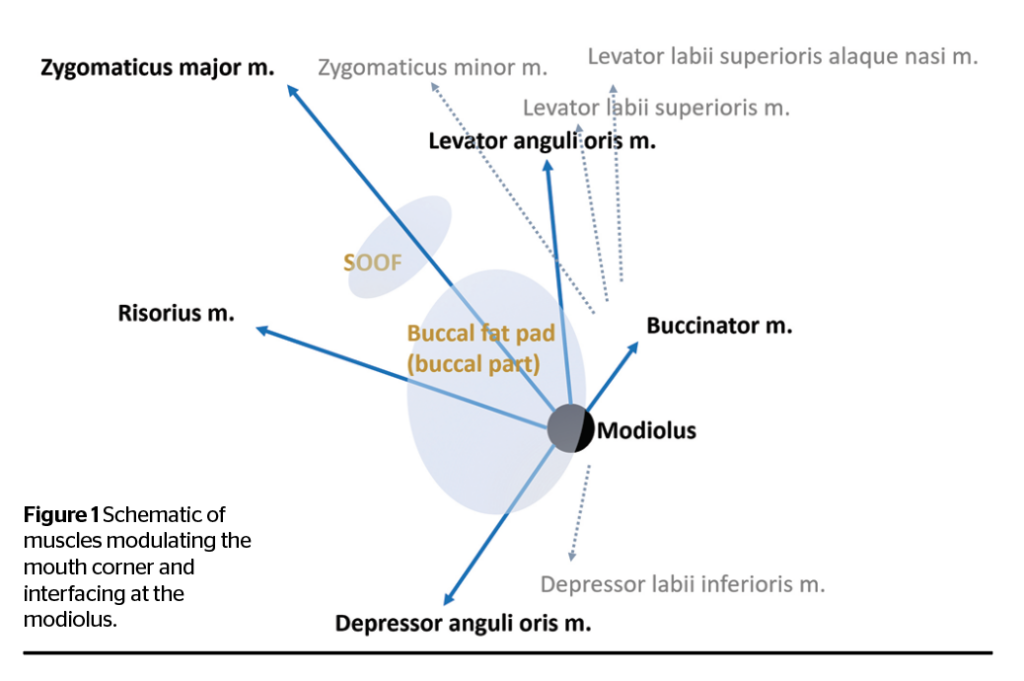
We devised an approach for the placement of HA fillers that allows the strategic direction of movements of the modiolus and perioral area. Our approach works synergistically with the modiolus’ constituent muscles while inhibiting antagonistic muscle movements (Figure 1). We report here the representative results from two patients treated with our injection strategy.
Materials and methods
Patients
Patients who presented with a downward mouth curvature and requested aesthetic treatments to correct this were enrolled. Patients were excluded from the study if they had a known allergic reaction to fillers, were undergoing anticoagulant or immunosuppressant therapy, had autoimmune disease, diagnosed psychological disorders like body dysmorphic disorder, or were pregnant or breastfeeding.
Patients’ faces were studied for the presence of drooping of buccal fat and mouth corners, deficient lateral suborbicularis oculi fat (SOOF) and lateral deep medial cheek fat pad (DMCF), and an overactive depressor anguli oris (DAO). To assess their suitability for perioral myomodulation, the zygomaticus major muscle (along the length of the upper margin of the temporal process) and the modiolus were palpated lightly by placing a finger on the temporal process to lift the area and allow soft tissue volume loss to be observed and estimated. Soft tissue above the DAO muscle was similarly estimated by palpating along the length of the modiolus and the oblique line of the mandible. Lips were assessed with patients in a seated position, who performed facial animations (including smiling, pursing lips, and expressing sadness) and facial relaxation (without clenching the jaw or teeth) to achieve a resting state. These actions allowed an estimation of soft tissue volume, as deficits here could also contribute to loss of lip contour.
Treatment
Anaesthetic EMLA® Cream 5% (lidocaine and prilocaine 1:1) was applied to the face 15 minutes prior to filler injections. Using 0.5-inch long, 27G and 30G needles (as supplied with filler; TSK Laboratory, Japan), the superior temporal septum and the temporal ligamentous adhesion were injected with a total of 1 mL of Belotero® Intense (Merz/Anteis SA, Geneva, Switzerland). The lateral SOOF and lateral DMCF were injected with a total of 2 mL of Belotero® Intense; the nose was straightened with injections of 0.5 mL of Belotero® Intense, and 1.5 mL of Belotero® Balance (Merz/Anteis SA, Geneva, Switzerland) was placed above the DAO. While 0.5 mL of Belotero® Intense was injected into the chin, and 1.5 mL of Belotero® Balance was superficially injected into the nasolabial fold and lip vermillion border. Specifically, filler was injected into the sub-SMAS beneath the orbicularis oculi, levator anguli oris (LAO), and levator labii superioris. With each injection point, small boluses (0.1–0.15 mL/point) were placed adjacent to strong ligamentous adhesions (the superior temporal septum, the temporal ligamentous adhesion, the lateral portion of the orbital malar ligament, and the zygomatico-cutaneous ligament) for structural support. Medium boluses (0.2–0.3mL/point) were placed in the lateral SOOF and DMCF to restore the lifting capacity of the levator muscles. Tiny boluses (0.05–0.1mL/point) were placed in the subcutaneous layer for aesthetic refinements. Due to the high vascularity of the perioral area, patients were monitored for adverse reactions like hematoma, ischemia or mottled skin for up to 30 minutes after injection. Post-treatment, patients were instructed not to massage the injected area and to keep the injection site dry and clean. They were also advised to avoid skin irritants or excessive sunlight exposure on the face for at least 1 week. To mitigate pain, they were advised to take acetaminophen for 3 days immediately post-treatment, as required.
Evaluations
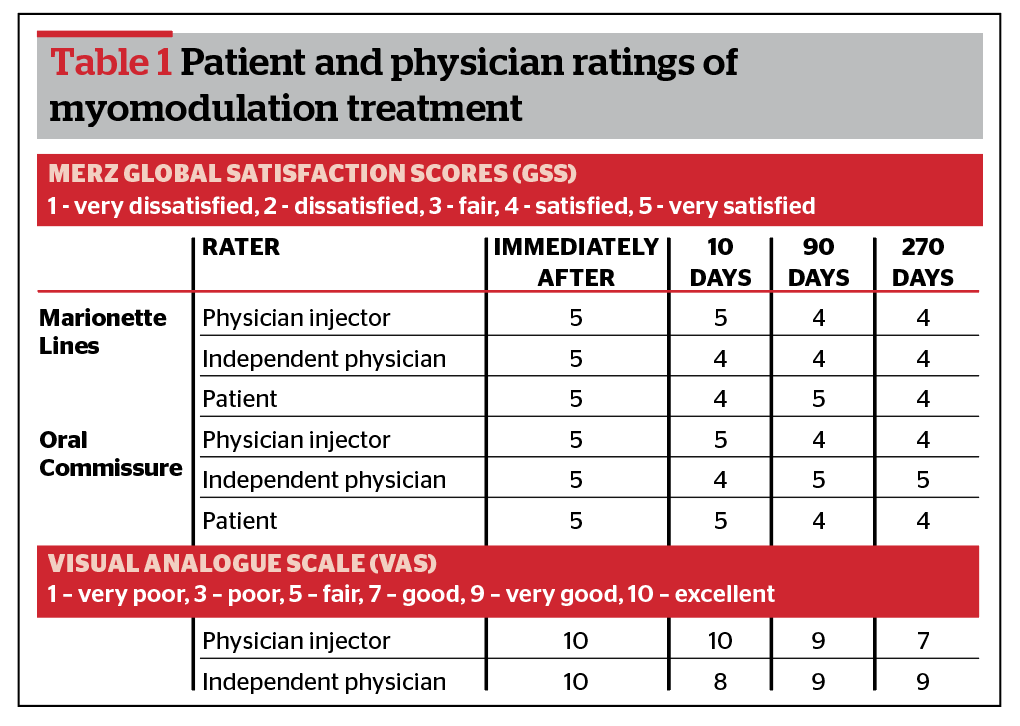
Patients were followed up at 10-, 90- and 270-days post-treatment. Evaluations included assessments of overall aesthetic improvements, lip contours, and positions of mouth corners (modiolus). The Merz Global Satisfaction Scale (GSS) was used to score the patients’, physician injector’s and independent physician’s satisfaction with treatment outcomes, while the physician injector and independent physician also scored satisfaction using the visual analogue scale (VAS).
Results
The representative outcomes of our HA filler-based perioral rejuvenation are demonstrated through a 36-year-old female patient (Figure 2). Overall, the patient demonstrated a younger appearance, a less pronounced downturn of the mouth corners, and less skin laxity in the treated area. Immediately post-injection, the perioral area appeared more balanced, while movement of the modiolus superiorly and posteriorly produced a more defined facial contour. Placing Belotero® Intense in the lateral SOOF and lateral DMCF elevated the modiolus while placing Belotero® Balance above the DAO blocked the modiolus’ downward and lateral traction force, resulting in midface lifting. Injections of Belotero® Intense in the chin aimed not to protrude the chin but to relieve mentalis strain and harmonise the whole face, while superficial injections of Belotero® Balance relieved the nasolabial fold and produced a more defined lip contour.

One 32-year-old female patient (data not shown) presented with a downturned lip contour due to a prominent right upper lip defect, a diminished overall lip body volume, and a volume-deficient superficial lateral lip suggesting a fat compartment deficiency above the DAO. Injection of Belotero® Balance (2 mL) elongated her lips and positioned the mouth corner laterally, restoring the lip contour and creating a more defined facial contour and a happier appearance. In general, the placement of 12 threads (9mL) of CaHA should lead to a visible facial ‘rejuvenation’, but in this patient, modiolus motion was not prominent due to the severity of bony loss and buccal fat herniation. All patients post-treatment demonstrated a more youthful and elevated facial appearance.
The results of our myomodulation strategy persisted at 270 days post-treatment, especially tissue lifting of the SOOF and DMCF at 90 days. The 36-year-old patient’s VAS and GSS (Table 1) ratings of their marionette lines and oral commissures were high, even up to 270 days post-procedure. We expect that the more severe the patient’s presentation, the more effective the myomodulation treatment will be. This patient’s result demonstrates that achieving effective myomodulation of mouth corners requires midface volume loss (especially in the SOOF), a supra-DAO deficit, a downturned mouth corner and skin laxity. Due to the limitations of improvements in the mobility of individual muscles, an effective filler dose of 6–10 mL should be used to ensure synergistic effects. Post-procedure, one patient experienced mild injection site swelling, and two patients experienced mild bruising. No hematomas or other adverse effects were noted, all of which resolved without requiring treatment. No severe adverse events occurred, and no patient required retreatments.
Discussion
Our patients had deficiencies in the lateral SOOF and lateral DMCF, which diminished the support typically provided by the zygomaticus major and LAO to the modiolus system, while an overactive DAO caused sagging of mouth corners. Our myomodulation approach enhanced the synergistic activity of the perioral muscles in which HA filler is placed while inhibiting their antagonistic activity, allowing us to control the direction of modiolus movement. The persistence of treatment outcomes at 180 days is encouraging as the highly-mobile perioral area resorbs filler the most, compared to other facial areas.
Perioral musculature is unique but complex due to a need to generate delicate movements for fine or subtle facial expressions. At least twenty muscles are involved in the myomodulation26 of mouth corners and are situated within a web-like structure comprising the complicated myodynamic system of the face. Multiple muscles insert into the modiolus, including the LAO, zygomaticus major, buccinator, risorius, depressor anguli oris and orbicularis oris27.
Like others13, our approach (Figure 3) considers facial muscle dynamics as part of a holistic functional unit encompassing muscle length, tension, synergism, and antagonism. Myomodulation outcomes may be variable due to static and dynamic changes that alter the structure and motion of the facial musculature and SMAS. Moreover, relative to skeletal muscles elsewhere in the body, the smaller facial muscles undergo a more subtle change following treatment. The modiolus system is surrounded by facial structures like the facial bone, buccal fat, superficial and deep fat compartment, and ligamentous tissue. Its mobility is thus also determined by the structures in which it is confined. Myomodulation is most optimal when treatment considerations include these factors, careful patient selection, and synergistic performance of aesthetic interventions.
Myomodulation may involve simple mechanical changes, stimulation of intramuscular cutaneous mechanoreceptors, and perhaps through filler-induced impairment of muscle movement. The concept of myomodulation originates from magnetic resonance imaging demonstrating that youthful facial convexity was due to deep fat compartments beneath levator muscles28, while age-related bone regression and fat loss were due to the loss of this convexity. Consequently, the levators straighten and have a stronger effect on depressor muscles13,22 so that loss of structural support can be restored by positioning fillers beneath the muscle and near its insertion point. This placement allows the filler to function as a fulcrum to restore tissue convexity and muscle tension13,23. However, we feel that this outcome depends on the area being treated and can be used successfully for the nasolabial fold. In the zygomaticus major, placement near the muscle origin creates a more vertically-positioned ‘apple cheek’, as fillers near the insertion lead to a heavy appearance. Conversely, muscle activity can be limited by the superficial placement of filler within the mentolabial angle or intramuscular placement within the periorbital or perioral sphincters19. In the perioral area, HA fillers may reduce lip elevation and restore muscular imbalances caused by structural deficiencies, regardless of volume loss13. Nasolabial fold myomodulation can be achieved by injecting filler near the point of skin insertion13.
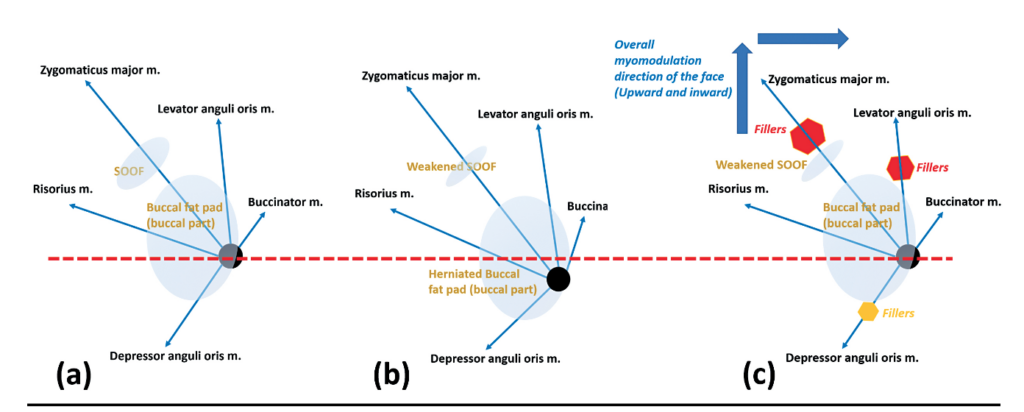
In another study20, volumising HA fillers injected into the SOOF were found to lift the midface, possibly because of the filler’s high G’ and cohesivity, which resisted migration and vertical pressures. Injecting fillers into the midface does not lift the SOOF as it is attached to the bone, but it does produce a myomodulating, midface lift as the filler causes a slight contraction of the striated orbicularis oculi muscle, which lifts the overlying superficial malar fat and its cutaneous sheath. This lifting of muscle anteriorly occurs even when very little filler (0.5 cc–1 cc) is placed in the SOOF, as long as the injected HA is in direct contact with the muscle or inside it. Myomodulation may also occur via HA filler-mediated muscle relaxation. HA filler-mediated nasolabial fold augmentation in the levator labii superioris facilitates myomodulation and relieves gingival show, while HA fillers in the orbicularis oris facilitate myomodulation of thin lips by relaxing muscle tension and skin tightness to restore a fuller lip.
Our procedure requires injection of HA fillers beneath the zygomaticus major, on the supraperiosteal layer, with caution exercised due to the presence of transverse facial arteries. Beneath the LAO, fillers should be injected in the sub-superficial muscular aponeurotic system (SMAS) layer, with caution exercised due to infraorbital and facial arteries or their branches in the area. Above the DAO, fillers must be injected precisely into the supra-SMAS layer. However, less-experienced injectors may inadvertently inject into the deep-SMAS to sub-SMAS layers, leading to suboptimal results or damage to the inferior labial artery. Perioral muscles are delicate structural layers interspersed with narrow spaces, especially in elderly patients.
Cannulas can be used to increase safety, but the perioral myomodulation by needle injection is superior, despite the risk of vascular events, because blunt cannulas only insert into up to four layers and will attenuate the subtle effects of perioral myomodulation. Aesthetic interventions in the perioral area are especially challenging due to the intricate anatomy and dynamic nature of the lower face29. To increase success in perioral myomodulation procedures, a comprehensive and thorough understanding of facial anatomy (particularly perioral musculature and vessel distribution), together with meticulous injection technique, is imperative. Gentle manoeuvring and filler injections also lower the risk of nerve injuries.
Cohesive HA fillers, like the Belotero® fillers, are recommended for the perioral area, as they give better tissue integration, more natural results, and few to no bumps or nodules30. However, others have noted that fillers with a moderate G’ and moderate cohesivity are also ideal for lip rejuvenation31,32. Fillers are less durable in highly mobile areas like the mouth due to high shearing forces that cause their degradation33,34, but it is essential to avoid harder or less-cohesive fillers that may cause complications like nodules1. Fillers that can cause the Tyndall effect are also best avoided in patients with Fitzpatrick Skin Type I–II with static perioral rhytids35.
Our study was limited by a lack of split-face or other controls to demonstrate the absence of myomodulation following filler injection. However, this would have been difficult to demonstrate as the muscles of the perioral area interface with each other so that myomodulating one functional, mimetic muscle group would have impacted others19. Due to its dynamic nature, video recordings of patients before and after myomodulation treatment would also allow filler-induced changes in muscle activity to be visualised more effectively19,24. We are currently also in the process of collecting long-term data on the durability of our intervention. Further study is needed to confirm the precise mechanisms by which myomodulation occurs and whether fillers affect muscle movements by weakening the underlying musculature or if they integrate subcutaneously to produce a lifting effect, especially in the middle third of the face24. Future work will include photographic quantification of outcomes, e.g., with QuantifiCare technology.
Conclusion
Facial volume restoration treatments typically achieve lifting in isolated areas due to the application of neurotoxins and facial fillers in discrete areas. Unlike neurotoxins, fillers can be used with high accuracy and produce durable outcomes, even in facial tissues with high mobility and complexity, such as the perioral modiolus system. As the perioral area should not be injected with high quantities of neurotoxins, which can lead to facial palsy-like appearances or an unbalanced face, our strategy was devised to achieve a holistic restoration of volume to the whole face. Moving the modiolus superiorly and posteriorly created a youthful and defined facial contour for our patients and showed that a precise and careful modulation of the modiolus system is key to effective perioral rejuvenation.
Declaration of interest Merz Asia Pacific Pte Ltd provided the study products and funds for editing of the manuscript by Dr Shawna Tan of Medical Writers Asia. Dr Tinchia Hsu was responsible for all study design, conduct, analyses, and manuscript review.
Figures 1–3 © Tinchia Hsu
Table 1 © Tinchia Hsu
References
- Sundaram H, Shamban A, Schlessinger J, Kaufman-Janette J, Joseph JH, Lupin M, Draelos Z, Carey W, Smith S, Eaton L. Efficacy and Safety of a New Resilient Hyaluronic Acid Filler in the Correction of Moderate-to-Severe Dynamic Perioral Rhytides: A 52-Week Prospective, Multicenter, Controlled, Randomized, Evaluator-Blinded Study. Dermatol Surg. 2022 Jan 1;48(1):87-93.
- Ali MJ, Ende K, Maas CS. Perioral rejuvenation and lip augmentation. Facial Plast Surg Clin North Am 2007;15:491–500, vii.
- Iblher N, Kloepper J, Penna V, Bartholomae JP, et al. Changes in the aging upper lip–a photomorphometric and MRI-based study (on a quest to find the right rejuvenation approach). J Plast Reconstr Aesthet Surg 2008;61:1170–6.
- Penna V, Stark GB, Voigt M, Mehlhorn A, et al. Classification of the aging lips: a foundation for an integrated approach to perioral rejuvenation. Aesthet Plast Surg 2015;39:1–7.
- Scarano A, Mortellaro C, Mavriqi L, Di Cerbo A. Evaluation effectiveness of the voltaic arc dermabrasion in perioral rhytides eradication. J Craniofac Surg 2016;27:1205–8.
- Ramaut L, Tonnard P, Verpaele A, Verstraete K, Blondeel P. Aging of the Upper Lip: Part I: A Retrospective Analysis of Metric Changes in Soft Tissue on Magnetic Resonance Imaging. Plast Reconstr Surg. 2019 Feb;143(2):440-446.
- Shah AR, Kennedy PM. The aging face. Med Clin North Am 2018;102:1041–54.
- Iblher N, Stark GB, Penna V. The aging perioral region—do we really know what is happening?. J Nutr Health Aging 2012;16:581–5.
- Sullivan PK, Hoy EA, Mehan V, Singer DP. An anatomical evaluation and surgical approach to the perioral mound in facial rejuvenation. Plast Reconstr Surg. 2010 Oct;126(4):1333-1340.
- Penna V, Stark G-, Eisenhardt SU, Bannasch H, Iblher N. The aging lip: a comparative histological analysis of age-related changes in the upper lip complex. Plast Reconstr Surg. 2009 Aug;124(2):624-628.
- Pascali M, Quarato D, Carinci F. Filling Procedures for Lip and Perioral Rejuvenation: A Systematic Review. Rejuvenation Res. 2018 Dec;21(6):553-559.
- Sayan A, Gonen ZB, Ilankovan V. Adverse reactions associated with perioral rejuvenation using laser, fat and hyaluronic acid: systematic review. Br J Oral Maxillofac Surg. 2021 Nov;59(9):1005-1012.
- de Maio M. Myomodulation with Injectable Fillers: An Innovative Approach to Addressing Facial Muscle Movement. Aesthetic Plast Surg. 2018 Jun;42(3):798-814.
- Carruthers J, Carruthers A, Tezel A, Kraemer J, Craik L. Volumizing with a 20-mg/mL smooth, highly cohesive, viscous hyaluronic acid filler and its role in facial rejuvenation therapy. Dermatol Surg. 2010;36(Suppl 3):1886–1892.
- Goldberg RA, Fiaschetti D. Filling the periorbital hollows with hyaluronic acid gel: initial experience with 244 injections. Ophthal Plast Reconstr Surg. 2006;22(5):335–341.
- Callan P, Goodman GJ, Carlisle I, Liew S, Muzikants P, Scamp T, Halstead MB, Rogers JD. Efficacy and safety of a hyaluronic acid filler in subjects treated for correction of midface volume deficiency: a 24 month study. Clin Cosmet Investig Dermatol. 2013;6:81–89.
- Jones D, Murphy DK. Volumizing hyaluronic acid filler for midface volume deficit: 2-year results from a pivotal single-blind randomized controlled study. Dermatol Surg. 2013;39(11):1602–1611.
- Harris S. Myomodulation, the mechanoreceptor-filler hypothesis [Internet]. PRIME Journal. 2019 [cited 2022Dec11]. Available from: https://www.prime-journal.com/myomodulation-the-mechanoreceptor-filler-hypothesis/
- Coimbra DD, Stefanello B. Myomodulation with Facial Fillers: A Comprehensive Technical Guide and Retrospective Case Series. Aesthetic Plast Surg. 2022 Nov 28. doi: 10.1007/s00266-022-03193-y. Epub ahead of print. PMID: 36443415.
- Belhaouari L, Tomassety M, Quinodoz P, De Boulle K. Myomodulation and hyaluronic acid [Internet]. PRIME Journal. Informa PLC; 2020 [cited 2022Dec11]. Available from: https://www.prime-journal.com/myomodulation-and-hyaluronic-acid/
- Cheng C, Cheng IT. Observation and Potential Mechanisms of Mentalis Myomodulation by Hyaluronic Acid Filler in the Treatment of Microgenia. Plast Reconstr Surg. 2021 Jun 1;147(6):1085e-1087e.
- de Maio M. Myomodulation with Injectable Fillers: An Update. Aesthetic Plast Surg. 2020 Aug;44(4):1317-1319.
- de Maio M. MD Codes™: A Methodological Approach to Facial Aesthetic Treatment with Injectable Hyaluronic Acid Fillers. Aesthetic Plast Surg. 2021 Apr;45(2):690-709. doi: 10.1007/s00266-020-01762-7. Epub 2020 May 22. Erratum in: Aesthetic Plast Surg. 2021 Feb 17;: PMID: 32445044; PMCID: PMC8012343.
- Kane MAC. Commentary on Myomodulation with Injectable Fillers: An Innovative Approach to Addressing Facial Muscle Movement. Aesthetic Plast Surg. 2018 Oct;42(5):1360-1363.
- Germani Vieira M, Rogerio V, Roschel P, Rabelo V, Teixeira T, Muñoz-Lora VRM. Myomodulation using hyaluronic acid fillers as an efficient and innovative treatment for gummy smile: A case report. J Oral Biol Craniofac Res. 2022 May-Jun;12(3):376-380.
- Kim HJ, Seo KK, Lee HK, Kim J. (2016). Clinical Anatomy for Botulinum Toxin Injection. In: Clinical Anatomy of the Face for Filler and Botulinum Toxin Injection. Springer, Singapore. https://doi.org/10.1007/978-981-10-0240-3_2.
- Dao DPD, Le PH. Anatomy, Head and Neck, Eye Levator Anguli Oris Muscle. [Updated 2022 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547688/?report=classic
- Le Louarn C, Buthiau D, Buis J. Structural aging: the facial recurve concept. Aesthetic Plast Surg. 2007 May-Jun;31(3):213-8.
- Varga R. Providing Optimal Rejuvenation to the Jawline and Perioral Area Using Neuromodulators and Hyaluronic Acid Dermal Fillers. Plast Surg Nurs. 2021 Apr-Jun 01;41(2):98-104.
- Prasetyo AD, Prager W, Rubin MG, Moretti EA, Nikolis A. Hyaluronic acid fillers with cohesive polydensified matrix for soft-tissue augmentation and rejuvenation: a literature review. Clin Cosmet Investig Dermatol. 2016 Sep 8;9:257-80.
- Wick EH, Ostby E, Grunebaum LD. Lip rejuvenation and filler complications in the perioral region. Plast Aesthet Res 2022;9:8.
- Fagien S, Bertucci V, von Grote E, Mashburn JH. Rheologic and Physicochemical Properties Used to Differentiate Injectable Hyaluronic Acid Filler Products. Plast Reconstr Surg. 2019 Apr;143(4):707e-720e.
- Carruthers A, Carruthers J, Monheit GD, Davis PG, Tardie G. Multicenter, randomized, parallel-group study of the safety and effectiveness of onabotulinumtoxinA and hyaluronic acid dermal fillers (24-mg/ml smooth, cohesive gel) alone and in combination for lower facial rejuvenation. Dermatol Surg. 2010 Dec;36 Suppl 4:2121-34.
- Küçüker İ, Aksakal IA, Polat AV, Engin MS, Yosma E, Demir A. The Effect of Chemodenervation by Botulinum Neurotoxin on the Degradation of Hyaluronic Acid Fillers: An Experimental Study. Plast Reconstr Surg. 2016 Jan;137(1):109-113.
- Micheels P, Besse S, Flynn TC, Sarazin D, Elbaz Y. Superficial dermal injection of hyaluronic acid soft tissue fillers:
comparative ultrasound study. Dermatol Surg. 2012;38(7 Pt 2):1162-1169.







