an aesthetic practitioner, Paris,
France
Catherine de Goursac discusses the available treatments to address signs of ageing in the hands, including chemical peels, lasers and cryotherapy
While the face and neck are very frequently the priority for rejuvenation interventions, the hands do not escape the effects of time, and often have the consequence of betraying one’s age. While the palmar side of the hand is functional, the dorsal side is visible and often reflects an individual’s age. The skin of the hands is particularly thin and fragile, containing few sebaceous glands (the glands that secrete sebum, a natural protective film for the skin). Furthermore, the hands are subjected daily to varying external aggressions, such as the sun, the cold, detergents, and frequent washing. Visible ageing on the hands can discredit a face that still appears young.
From the age of forty, or even earlier in some people, solar lentigines (also known as liver spots, brown spots, sun spots or age spots) gradually begin to appear on the hands and can present all over the dorsal surface of the hands and fingers, often more numerous on the hand that is more exposed. The skin of the dorsal surface of the hand and the fingers becomes dehydrated and thin with laxity appearing due to lost tonicity.
“It is now possible to rejuvenate and beautify the appearance of the hands, thus avoiding the unsightly contradiction between a maintained face and ageing hands, which, left untreated, can betray one’s age.”
After the age of 50, the venous network of the hand becomes increasingly apparent and the tendons begin to protrude. As the interosseous muscles shrink, the amount of subcutaneous fat decreases and the underlying bone structure becomes visible. This phenomenon, known as skeletonisation, eventually leads to a gaunt and bony appearance in the hand(1).
While ageing of the hands occurs in both men and women, requests for rejuvenation come predominantly from women, although the percentage of male clientele is increasing annually as men begin to become more concerned and take better care of their physical appearance.

Aesthetic medicine has expanded considerably in recent years, bringing together a set of non-invasive, non-surgical medical procedures that can be performed on an out-patient basis in the medical office, with no downtime, and which have proved their value. With these advances, it is now possible to rejuvenate and beautify the appearance of the hands, thus avoiding the unsightly contradiction between a maintained face and ageing hands, which, left untreated, can betray one’s age. The techniques currently available are diverse and can be combined or used in monotherapy, according to the patient’s needs. The choice of the most appropriate treatment method depends upon the practices and preferences of each practitioner.
The modern therapeutic arsenal currently available to practitioners meets the growing demand of patients wishing to rejuvenate ageing hands. In this article, the author will focus on the medical procedures utilised in their practice to treat the frequently associated clinical signs of ageing hands:
- The appearance of dark spots on the backs of the hands and the fingers
- The appearance of wrinkles on the skin surface caused by thinning cutaneous tissue
- Skeletonisation or an emaciated appearance on the dorsal surface of the hands
- Visible veins.
Causes and risk factors
Skin ageing is the consequence of a conjunction of the intrinsic or chronological ageing process and the extrinsic processes that influence ageing via multiple environmental or external factors:
- Age-related intrinsic or chronological ageing is the inevitable process determined by genetic inheritance and hormones (oestrogen reduction during the menopause) that cannot be avoided
- Extrinsic ageing can be considered as ‘lifestyle’ related ageing.
- Each day, the hands are exposed to multiple external aggressions, including:
- The sun, first and foremost, is responsible for photo-ageing, along with artificial UV tanning practices. The weathered skin seen on sailors or mountaineers is representative of the effects of excessive exposure to solar radiation
- Climatic and temperature variations: wind, cold, and heat
- Mechanical aggressions such as friction, pressure, and repeated shocks
- Toxic-chemical aggressions: tobacco, household/cleaning products, and air pollution
- Microbial aggressions: germs from soiled surfaces such as toilet bowls, subway and bus ramps, television remote controls, computer keyboards, etc.
- Hard water with a high percentage of limestone (calcium). The surface hydrolipidic film (the acid mantle) on top of the epidermis, composed of water (perspiration) and lipids (sebum), provides a barrier between the outside world and the skin. Repeated hand washing with hard limestone water alters this film and weakens the non-pathogenic microbial flora essential for skin protection.
All these factors prematurely age the hands, and particularly as the skin of the hands is thin, fragile, and frequently photo-exposed, can give the hands an unsightly appearance.
“Moisturise the hands regularly with a product specifically rich in moisturising and softening agents, particularly before bed, as sleep is the most productive time for cutaneous regeneration.”
Prevention of skin ageing: best practices
The author provides their patients with some elementary measures to reduce the impact of extrinsic factors that lead to premature ageing of the hands:
- Avoid sun exposure when they are without appropriate sun protection, even in winter, especially in persons with light-coloured skin (UV tanning salons should equally be avoided)
- Moisturise the hands regularly with a product specifically rich in moisturising and softening agents, particularly before bed, as sleep is the most productive time for cutaneous regeneration. Patients may apply their cosmetic face, neck and hand cream. Although the hands are frequently neglected during the daily beauty routine, the hands should receive just as much care as the face
- Wear protective gloves to avoid contact with water that is too hot or hard, cleaning products that are corrosive or harsh and when washing dishes and performing other household chores. Wearing gloves when going outside should also be a regular habit
- Wash the hands in a pH neutral soap or with a cleansing oil
- Limit the use of antibacterial gels as they contain alcohol, which dries the skin.
Medical management of hand ageing
An initial consultation is essential before any therapeutic intervention in order to verify that the patient meets the feasibility criteria for the aesthetic treatment. The physician carries out a detailed investigation followed by a careful clinical examination to ensure the absence of contraindications, which, being well known to practitioners, will not be detailed here. At the end of this consultation, the patient is given a fact sheet on the protocol, and the cost of the procedure is determined. These medical treatments require free, informed, written and signed consent from the patient.
There is no one standardised procedure for the treatment of ageing hands; rather, each patient is treated as a unique case that requires appropriately tailored care.
Several criteria are taken into account in order to guide the choice of treatment. These criteria are medical: cutaneous phototype, number and appearance of the lesions, ageing evolutionary stage, possible side-effects, and clinical experience of the practitioner. There is also the patient criteria to take into account, such as the age of the patient, his or her preferences, his or her expectations (realistic or not), and treatment cost.
The author will now outline their practical approach to the care of ageing hands. This intervention involves four steps, often overlapping. However, for the sake of clarity, they are described below in succession.
- Remove or fade dark spots on the hands and fingers
- Restore volume to the back of the hands to reduce a gaunt appearance
- Improve the quality of the skin
- Decrease the diameter of the veins that are becoming more visible.
Dark spots on the back of the hands and fingers
The primary cause of the appearance of dark spots is sun exposure and/or artificial tanning. Brown spots may appear earlier in fair-skinned people after a severe sunburn or repeated sun exposure. These actinic or solar lentigines are more numerous in photo-exposed zones; for example, the left or right hand of automobile drivers or the right hand of golfers (the left usually being protected by a glove).

Another factor increasing the appearance of dark spots is the intrinsic ageing process that causes senile lentigines or age spots.
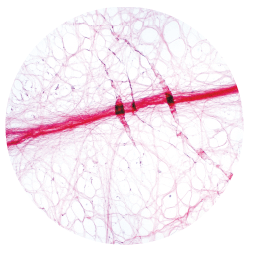
This hyperpigmentation localised on the surface of the epidermis is the consequence of an accumulation of melanin (the pigment synthesised by melanocytes that determines skin colour). These spots are flat, smooth, painless, of varying sizes, and brown in colour in contrast to the surrounding lighter coloured skin.
“The trichloroacetic acid peel (TCA) is the peel of reference in medical aesthetics, due to its universal usage for many years, flexibility, and relatively inexpensive cost.”
These lesions are benign, and if diagnosed as such by the physician, require no treatment except from an aesthetic point of view for which they are a common reason for consultation. Actinic keratoses, given their particularities, will be discussed at the end of this section.
Rejuvenation of the hands begins with the treatment of dark spots. To begin with, the physician conducts a careful clinical examination of the pigmented spots to confirm that they are benign. The choice of the most suitable treatment is for the physician to decide, who will treat the patient according to their phototype.
The author offers widely-recognised therapeutic solutions, such as chemical peels, lasers or cryotherapy. All these techniques leave small crusts or scabs that fall off within a few days, revealing the smooth, treated skin. It is very important not to pick these crusts, which could leave a scar.
The 15% TCA chemical peel for all phototypes
Chemical peels are indispensable tools in the therapeutic arsenal of the aesthetic doctor(2). This treatment is performed in the medical office by a trained operator.
The trichloroacetic acid peel (TCA) is the peel of reference in medical aesthetics, due to its universal usage for many years, flexibility, and relatively inexpensive cost.
Trichloroacetic acid, a trichloro derivative of acetic acid (vinegar acid), is non-toxic and non-allergenic. The intensity of its effect is adjustable via the concentration used (the higher the concentration, the stronger its action), as well as the amount deposited (number of layers). This keratolytic agent produces an action in two stages:
- The first stage eliminates the stratum corneum layer located on the surface of the epidermis, colonised by pigment deposits
- The second stage leads to skin regeneration by stimulating collagen synthesis via growth factors.
Several laboratories or distributors offer TCA peels available in different formulations and at different concentrations of acid. Without being exhaustive, some of the products selected by physicians are from the following laboratories: Dermaceutic (Cosmo Peel), Mene & Moy (now Eneomey), Novelskin® (PRX-T33) and Innoaesthetics (Mg-TCA 35 now known as MCA 35).
In the author’s experience, they prefer to use the Easy TCA® peel (Skin Tech Pharma Group S.L., Costa Brava, Spain). Easy TCA®, created by Dr. Philippe Deprez, is a TCA chemical peel with a 15% concentration, which can only be administered by a trained physician(3). This patented technology has CE marking 1014.
Two reasons motivate this choice of product:
- The first reason is the product composition. The concentration of TCA is fixed (15%) as its formula is pre-established. The 15% is added extemporaneously to a base solution containing adjuvants such as AHAs (Alpha-Hydroxy-Acids or fruit acids), vitamins, saponins and antioxidants (minimising the risk of pigment rebound). The TCA is thus stabilised, allowing homogeneous penetration on the whole of the skin, and limiting the risk of side-effects.
- The second reason is the treatment protocol. Treatment of the facial area is one of the most common requests, and for this indication, the desired frosting of the treated area is a homogeneous white (whitening of the epidermis via the coagulation of proteins). In contrast, using the peel on the hands requires good mastery of the degree of frosting for the following reasons: the process of frosting of the skin is somewhat longer to obtain, and it is imperative to stop the action of the TCA as soon as a white pattern (flakes of frosting) appears on the surface of the skin. Healing the skin of the hands is more difficult due to the absence of cutaneous appendages. It is important not to wait for complete blanching, otherwise you will have poor healing and a risk of unsightly scarring. In practice, the physician applies the peeling solution by cotton swab to target the affected area with precision. Application of the product needs to be repeated several times during the same session because the skin of the hands reacts more slowly to TCA 15%. As soon as the treated area of the hands begins to whiten, the peel is finished, unlike other areas of the body where complete frosting is needed for effectiveness. Sometimes the author uses a deeper trichloroacetic acid, such as Skintech’s Unideep peel or Only Touch for the treatment of lentigines. During the application, a tingling or burning sensation is felt by the patient, but is bearable and does not require anaesthesia. As soon as the desired degree of frosting is obtained, the action of the TCA is stopped by the application of compresses soaked in water.
The immediate effect is the appearance of light blanched spots on the skin that take a pink colour for a few hours and then stabilise to a brownish-pink colour. The treated areas will peel lightly for a few days.
To safely and effectively treat pigmentation spots, the peel, performed in the physician’s office, should be repeated twice (with approximately 10 days between sessions). Following this protocol, pigmentary reactions are extremely rare. It is, therefore, suitable for all phototypes I to VI. Exposure to the sun is strictly prohibited following the treatment and it is essential the patient applies a total protection sunscreen to the treated area.
To fade areas of diffuse pigmentation, we prescribe RegMain cream (Laboratoires Pech Cerciat, France), composed of natural ingredients (micro-algae and plant extracts), 2 to 3 applications per day massaged into the back of the hands, emphasising the liver spots, and protective sunscreen.
Laser treatment according to the patient’s phototype
For light phototypes (I to III), two types of lasers treat dark spots, either through abrasion or through a photomechanical method.
Fractional CO2 laser
The fractional carbon dioxide (CO2) laser has a partial abrasive action on the skin to eliminate solar lentigines or age spots. Targeting the water contained in the skin, this technique consists of creating non-contiguous micro-zone skin ablations in the affected area, leaving healthy skin at intervals between each ablation, from which healing will proceed more quickly. Its indications are reserved for patients with a light phototype because on darker phototypes it carries a risk of pigmentary rebound.
The Alexandrite 755 nm laser mainly targets eumelanin (brown-black pigment). The laser will, therefore, be effective only if the spots targeted are quite dark, as the laser radiation captures this colour. The energy produced by this laser causes an intense photomechanical impact that fragments melanin into microparticles, without any abrasive effect on the skin. These micro-fragments are then naturally eliminated by the body. The ideal situation for this type of treatment is the combination of a light phototype with spots that have a fairly high concentration of melanin. Our centre is equipped with the latest generation Alexandrite laser, which increases the efficiency and safety of treatment while preserving patient comfort.
Redheads have the unique trait of producing pheomelanin, a particular type of melanin that absorbs very little laser energy. Spots on this type of skin can not be effectively treated by laser.
Laser interventions require precautions to be taken before, during, and after treatment:
- The skin should not be tanned before the session.
- Self-tanning and tanning booths are to be prohibited.
- Treated skin must be protected from the sun with a high-index sunscreen during and after the treatment for the period of time recommended by the doctor.
“Dark skins age better and slower because they are naturally high in pigmentation but they are also prone to pigmentation disorders. This type of skin tone can be affected by the harmful effects of the sun. “
For dark phototypes (IV to VI)
The particularity of black, brown or mixed skins compared to light skins is due to the higher concentration of eumelanin present in the skin. Dark skins age better and slower because they are naturally high in pigmentation but they are also prone to pigmentation disorders. This type of skin tone can be affected by the harmful effects of the sun. Black skin is not without risk of burns (sunburn) and sun lentigines, especially on the face and hands, even if they are rare. Age can simply lead to a disruption of the melanin production and distribution mechanism. During sun exposure, black and brown skin requires adequate sun protection to avoid the stimulation of eumelanin, which may cause the appearance of dark spots.
To eradicate pigmentary lesions on dark phototypes, the author is using a specific new-generation laser: the Q-Switched Nd:YAG laser. Its 1064 nm wavelength is poorly absorbed by the melanin but it ensures deep light beam penetration, which destroys the abnormal pigment (spots), while generally respecting the natural pigmentation of the skin. This laser fragments the pigment via photo-acoustics (shock waves) and not by thermodynamics (which would cause a post-laser inflammatory reaction)(4,5).
Under current French regulations, the use of these rather powerful laser devices is reserved only for experienced laser physicians due to the potential dangers, such as skin burns caused by incorrect laser parameterisation. Wearing safety goggles is essential for the duration of the laser session to avoid damage to the eyes. The number of sessions and the interval between each session necessary to produce the desired results is determined by the treating physician.
“Cryotherapy, or extreme cold therapy, is performed with a cotton swab soaked in liquid nitrogen and applied directly to each spot. The cold freezes the surface layer of the skin, creating a thermal shock. “
Even though Q-Switched lasers are widely regarded as the standard treatment for pigmented lesions, post-inflammatory hyperpigmentation (HPPI) can complicate this aesthetic procedure. Patients should be informed of this potential risk. These pigmentary alterations can occur in all types of skin and at any age, but they particularly affect people with dark phototypes(6,7). Hyperpigmentation is a reactive hypermelanosis secondary to endogenous inflammation, such as acne, atopic dermatitis and contact dermatitis or skin trauma (even minor wounds, picking at pimples, insect bites, cuts or burns) or can be iatrogenic (caused by lasers, for example). Hyperpigmentation usually manifests as hyperpigmented macules that persist for weeks or even months without treatment. Laser technology is not indicated to remedy this reaction. On the contrary, it could lead to an increase in pigmentation following the transient inflammation caused by laser firing.
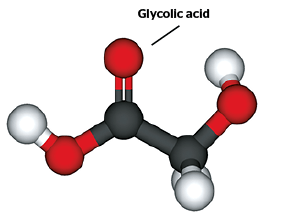
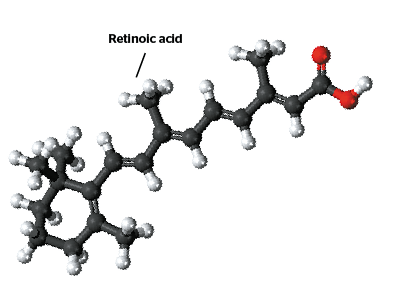
In these cases, the author prescribes depigmenting agents in the form of topical compositions that act on the synthesis of melanin in order to slow down production to reduce these spots. These products are based on retinoids derived from vitamin A, vitamin C or glycolic acid. Sun protection is essential.
The use of local corticosteroids is extremely common(7). Apart from a few exceptions, we do not prescribe local corticosteroid therapy, because the management of these pigmentation disorders lasts for a period of several weeks, and the regular application of corticosteroids is not, in our opinion, a good indication as it involves risks of corticoid-induced cutaneous atrophy.
Cryotherapy
Cryotherapy, or extreme cold therapy, is performed with a cotton swab soaked in liquid nitrogen and applied directly to each spot. The cold freezes the surface layer of the skin, creating a thermal shock. It is a therapeutic method that is simple, fast, efficient, inexpensive, and does not require anaesthesia when there is a fairly limited number of lesions. Cryotherapy can induce hypochromia if applied too deeply, especially on black skin. The treated areas must be protected by sunscreen.
” The aim of the PDO threads is to redensify the dermis by stimulating the fibroblasts, as well as a slight tightening effect
to correct moderate skin slackening.”
To conclude the discussion on cryotherapy, the author will consider the particular case of actinic, solar or senile keratoses. Actinic keratoses (AK) present as variably coloured plaques (brown, red, greyish), variable in number and thickness, covered with fine scales and rough to the touch, which appear on the back of the hands and fingers. They more often affect people with a light phototype who have chronic sun exposure, either from their leisure time or their professional activity (especially men working in an outdoor occupation: sailors, farmers, construction workers, etc.). Untreated AK can persist, spontaneously regress, or develop into squamous cell carcinoma. AK is, therefore, not solely an aesthetic problem, and, as they are considered precancerous lesions, should be treated by an experienced physician. Typically, the physician is able to make a diagnosis by a simple physical examination. If in doubt, a skin biopsy is required to determine the diagnosis with certainty. Early diagnosis for AK is important in order to implement a treatment that is both curative and preventive.
The major goal of curative treatment is to prevent the risk of malignant transformation.
Several therapeutic options are available to destroy these lesions.
- Cryotherapy represents the reference treatment for AKs in our clinical practice when the keratotic lesions are of a moderate thickness to cause a thermal shock that will destroy them
- Electrocoagulation or thermo-coagulation is a possible alternative in the case of thicker lesions. This medical technique involves placing an electrode with a small round extremity of a few millimetres in diameter through which passes a brief electrical current (heat) on the area to be treated. This results in the localised destruction of the target tissue on contact. This technique is fast and effective, but is quite painful and therefore requires local anaesthesia
- Lesion vaporisation by CO2 laser may also be a therapeutic option. This technique is effective but expensive.
Following treatment, annual monitoring is necessary to detect and treat any new lesions or any possible permutation of an existing lesion into a malignant cutaneous lesion.
Prevention is key. The main measures include avoiding sun exposure and artificial UV radiation related to tanning booths, especially for patients with light phototypes and/or occupational exposure to UV (sailors, farmers, etc), as well as effective photo-protection against UVB and UVA exposure through the regular use of high index sunscreens.
Treating skeletonisation of hands that appear bony or gaunt
Dermal fillers must have a number of qualities that allow the doctor to use them without risk: CE marking, biodegradability, biocompatibility according to ISO standards, non-animal origin, easy to inject, well-tolerated, and long efficiency (1–2 years). Today there are a large number of fillers, each with its own chemical constituents, indications, and effectiveness.
Hyaluronic acid (HA) is a reference product in medical rejuvenation due to its hydrating capacity from its hygroscopic properties, significant volumising capacity depending on the cross-linkage, and biological capacity via stimulation of fibroblasts activity (collagen synthesis), inducing tissue remodelling. HA is widely used for hand rejuvenation(8–10). Khosravani et al. (2019) published their technique for administering Restylane® Lyft Lidocaine (cross-linked hyaluronic acid gel 20 mg/ml replacing Perlane®) from Galderma laboratory to rejuvenate the hands effectively and safely. This is the first HA-approved injectable filler approved by the US Food and Drug Administration (FDA) in 2018 to restore volume to the dorsal surface of the hands. We, therefore, use this filler primarily for the same indication, to restore lost volume, improve cutaneous trophicity and reduce the visibility of veins and tendons. We elect to use two types of HA: Juvederm Ultra 4 and Restylane Volyme, available as sterile and disposable prefilled syringes containing lidocaine, with sterile 27G 1/2 needles.
The author’s administration protocol is as follows:
- Before injecting these products, the author dilutes them in physiological saline. Diluting the HA with physiological saline allows the author to increase the volume injected, and to obtain a better filling of the back of the hands at a lower cost. The physiological saline is trapped in the meshes of hyaluronic acid and does not reabsorb quickly
- Despite the presence of an anaesthetic in the syringes, the author first administers a local anaesthesia limited to the skin entry points (2 to 3 approximately) in the interdigital spaces to ensure total desensitisation
- The cannula is then slowly introduced into the dermis from these points of entry
- The content of the syringe is administered slowly using the linear retractor technique, which ensures a homogeneous and even distribution of the filler
- Juvederm Ultra 4 (Allergan Laboratories, France) is a cross-linked hyaluronic acid gel (24 mg/ml). The prefilled 1.0 ml syringe is diluted in 1.5 ml of saline. After dilution, the final volume injected into the dermis of each hand is 2.5ml
- Restylane Volyme (formerly Emervel Volume) from Galderma, France, is a cross-linked HA gel (20 mg/ml). Before the procedure, the prefilled 1 ml syringe of Volyme is diluted in 2 ml of physiological saline. The total volume injected is 3 ml per hand.
The benefits obtained from the injection last for approximately one year and can be maintained at the request of the patient, as these biodegradable products provide a temporary correction.
Management of the appearance of the skin of the back of the hands and the knuckles
The backs of the hands
As carboxytherapy, mesolift, radiofrequency, and chemical peels are techniques well known to practitioners specialised in aesthetic medicine, and frequently used in association with each other, the author will not review these treatments here.
The introduction of bio-resorbable medical polydioxanone (PDO) threads is not yet common practice for this indication. The author currently offers patients the opportunity to benefit from this new therapeutic approach stemming from their personal experience(12,13).
“In our practice, we recommend RegMain® anti-ageing hand cream or depigmenting products, available in a serum or cream formula and containing retinoic acid (an active derivative of vitamin A), glycolic acid or vitamin C.”
The aim of the PDO threads is to redensify the dermis by stimulating the fibroblasts, as well as a slight tightening effect to correct moderate skin slackening.
The author elects to use the Korean PDO Basic type wire for this indication. These ultrafine threads, straight and with a smooth surface, are inserted in parallel or in a subcutaneous mesh in the region to be treated. For the comfort of the patient, a small local anaesthetic via injection is administered at the points of entry of the threads. Each wire is then inserted into the subcutaneous space, one by one, through a fine needle. The needle is then removed, and the thread is left in place. On average, the author implants 10 wires per side.
The knuckle area
With time, the skin that covers the dorsal surface of the fingers facing the phalanges dehydrates and creases, forming wrinkles. There is currently a large demand from our patients to correct this unsightly problem. In response, we practice mesotherapy or mesolift sessions or anti-age revitalisation to improve the quality of the skin and rehydrate the dermis. Micro-injections of products adapted to the needs of the patient are administered to the dermis via an injection gun. This cocktail of personalised active principles is composed of vitamins (in particular A and E), trace elements with antioxidant properties (zinc, selenium) and non-reticulated hyaluronic acid with moisturising properties without creating volume at the injected area, for particularly dehydrated skin. An anaesthetic cream is applied to the areas to be treated one hour prior to the intervention to render the treatment painless. The treatment programme consists of approximately five sessions, spaced one month apart, with an annual maintenance session. Throughout the sessions, the skin becomes firmer and smoother.
Treatment of prominent veins on the dorsal side of the hands
The injection of fillers attenuates the appearance of visible veins on the back of the hand. However, there is a growing demand to treat the dilated and sinuous appearance of superficial dorsal veins, visible through the epidermis, and resulting from a loss of elasticity in the venous wall, which present a genuine aesthetic concern. These veins are not, strictly speaking, varicose veins. Their treatment is purely aesthetic.
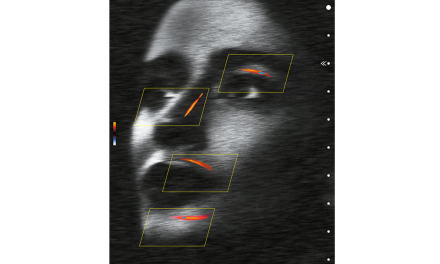
Currently, we recommend the percutaneous Nd:YAG laser treatment in the management of the most prominent veins. At the present time, the most suitable laser is the latest generation Nd:YAG laser that emits a wavelength of 1064 nm. The blood vessel to be treated is approached transcutaneously. Traversing the skin without damaging it, the laser beam will be absorbed by the oxyhaemoglobin contained in the vein, and the light energy of the laser beam is converted into heat. This locally generated heat causes a retraction of the vein, which results in a reduction of the vascular calibre.
Before each session, the doctor determines the optimal laser parameters: fluence (J/cm²), spot diameter, and pulse duration. Laser pulses are then delivered on the path of each target vessel. Pain is common during the session but anaesthesia is not recommended as it causes vasoconstriction, making the treatment less effective. The use of a skin cooling system helps to reduce pain. A dark phototype is not an obstacle to this laser due to its good depth of skin penetration, poorly absorbed by the melanin contained in the skin. The treatment often requires two sessions spaced a few weeks apart. A study published in 2012 by dermatologist Dr. Larrouy suggests the effectiveness of Nd:YAG long pulse treatment on the reduction in diameter and visibility of the superficial dorsal veins of the hands administered in two sessions carried out in 4 to 6-week intervals(14).
Discussion
Aesthetic medicine includes a wide range of non-invasive, out-patient techniques for hand rejuvenation that correct the signs of ageing, such as dark spots, a scrawny or gaunt appearance, wrinkles on the backs of hands and the knuckles, and prominent veins, with natural and durable results. The choice of the most appropriate treatment for each patient is specific to each physician and influenced by his experience and preferences.
The treatment of dark spots is frequently the first aesthetic treatment request for an office visit. Once diagnosed as benign by the clinician, the author offers three aesthetic treatment options for dark spots: chemical peels, laser or cryotherapy. The chemical peel is the gold-standard treatment in the management of dark spots. The author’s preference is for the Easy Peel®, at a concentration of 15%, administered per the protocol described above. A recent study (2017) published in JAMA shows that when the product is correctly applied, TCA peels are effective, safe and suitable for any phototype, with a low risk of complications(15).
The treatment of dark spots (solar lentigo and certain brown pigmentation) by laser appears to be a consensus. They are preferentially treated by the 755 nm Alexandrite laser for light skin (phototypes I to III) and the Nd:YAG 1064 nm laser for dark skin. These lasers are very effective for eliminating them in very few sessions.
However, the author will also mention some clinical studies published in recent years with other laser devices or IPL (Intense Pulsed Light), giving satisfactory preliminary results. Kung et al. obtained good results with the double-wavelength (532 nm and 1064 nm) picosecond laser, a combination of the Alexandrite and the Nd:YAG lasers for the treatment of benign pigmented lesions on Asian skin with low risk of post-inflammatory hyperpigmentation. This study involved 12 cases of phototype III to IV(16).
Friedmann et al. conducted a prospective single-centre study of 16 Caucasian women, mean age 55 years, with solar lentigines on the face and hands. The authors concluded that IPL treatment with a KTP (potassium-titanyl-phosphate) laser filter emitting a wavelength of 525-585 nm is effective and well-tolerated to significantly reduce these spots(17).
In 2015, Schoenewolf et al. showed superior efficacy of the Q-switched ruby laser (694 nm), which acts by photomechanical effect, vs an ablative fractional CO2 (photo-thermolysis) laser in the treatment of solar lentigines on the back of the hands in a study involving 11 patients(18). The main limitation of these studies is the small number of subjects used.
Many cosmetic products are available to regulate pigmentation. Most rely on key ingredients that act on the synthesis of melanin to help slow down melanin production. In our practice, we recommend RegMain® anti-ageing hand cream or depigmenting products, available in a serum or cream formula and containing retinoic acid (an active derivative of vitamin A), glycolic acid or vitamin C.
These non-prescription topical products necessitate the regular use of full sunblock at each occasion of sun exposure. However, there is little clinical data that have demonstrated the effectiveness of such an approach. These treatments can be used for many purposes: prevention, treatment for light-coloured spots and as an adjunctive to an aesthetic treatment to improve and maintain the results of the medical procedure.
Some studies referenced in the PubMed database have shown good results in small trials. Among these studies, the author will mention three relatively recent articles concerning the beneficial effects of certain topicals on the photo-ageing of the hands: a study by Roberts et al. of Rejuvaphyl® Hand and Neck Complex Cream (MD Rejuvena, Inc., California); Schlessinger et al. study of Marini ReNu Corrective Hand Complex (Jan Marini Skin Research, Inc.); and a study from Gold and Gallagher highlighting the benefits of the Vivité Vibrance Décolleté Cream (Allergan, Inc)(19–21).
Finally, the particular case of actinic keratoses, which, in the absence of effective treatment, can evolve into cutaneous carcinomas, is considered to be a curative treatment. The treatment objective is the destruction of the lesions, followed by regular post-treatment monitoring for possible recurrence or malignant permutations. The available therapies for actinic keratoses are: cryotherapy, electrocoagulation, and CO2 laser. When the lesions are few in number, the reference treatment is simple, fast, technical cryotherapy that does not require specific equipment. If in doubt, a skin biopsy should be performed.
When there are multiple lesions, the CO2 laser, and especially electrocoagulation, can be treatment options. The CO2 laser should be used with caution in the elderly as healing is more difficult and lengthy for seniors.
Prescription topical medicinal products such as 5-fluorouracil (5-FU) cream are prescribed by some clinicians for the treatment of actinic keratoses(22,23). Generally, these treatments are lengthy and generate frequent undesirable cutaneous side-effects. This medical intervention is not part of the aesthetic repertoire that the author practises in their centre, as with surgical excision when necessary.
Post-inflammatory hyperpigmentation (HPPI) sometimes complicates cosmetic procedures, such as high-concentration peels or laser-induced skin injury(24). Post-inflammatory pigmentations generally recede in a few weeks to a few months, but may nevertheless justify interventions that are mainly chemical treatments using topical depigmenting agents (derivatives of vitamin A, vitamin C, etc.) or specific peels. The author avoids using laser, a source of cutaneous physical aggression, for depigmentation. The scrupulous use of photo-protection is recommended.
Brown spots have long been treated by cryotherapy. This procedure has two major advantages: efficiency and low cost compared to other treatments.
Todd et al. conducted a comparative study of three laser devices versus cryotherapy on 27 cases with multiple solar lentigines on the back of the hands. For the authors, the efficacy of laser treatment was superior to that of cryotherapy(25).
Referring to the literature, two major types of fillers are commonly used for hand rejuvenation and reduce the visibility of veins and tendons: the more or less cross-linked hyaluronic acids and calcium hydroxylapatite (CaHA) marketed under the name of Radiesse® (Merz Aesthetics)(26,27).
Many studies have demonstrated the efficacy and safety of Radiesse® (synthetic calcium hydroxylapatite microspheres suspended in an aqueous gel) to plump the dorsal surface of the hands; the most recent of which are cited(28–30).
“A pilot study was conducted by Hoevenaren et al. to analyse the ageing process of the hand with three-dimensional stereophotogrammetry. This non-invasive 3D imaging technique offers the possibility to visualise the precise areas of volume loss of the dorsal surface of the hand, to identify the treatment areas and to evaluate the results obtained objectively and comparatively.”
The author’s preference, however, is for hyaluronic acid (HA). Radiesse® does not attract and hold water and is not immediately soluble in water, unlike HA fillers. Radiesse® injections are slightly less volumising, but the hydroxylapatite particles will induce an important stimulation of endogenous collagen synthesis by activation of the fibroblasts until their complete dissolution. One of the main advantages of Radiesse® is its longevity; it features a lasting result of between eighteen months and two years. Radiesse® is included in the author’s injectables offer, if the patient wishes.
With ageing, the skin of the back of the hand becomes slackened, thin, creased, with wrinkles or fine lines appearing. Carboxytherapy, mesolift, radiofrequency, and chemical peels are advanced medical techniques widely used in aesthetic procedures. Currently, we also offer patients the opportunity to benefit from the insertion of bio-resorbable medical PDO wires. Our experience in this field has led us to extend the possibilities offered by this non-invasive technique to the hands and thus expand our therapeutic range. This is a promising method, currently being carried out in our centre.
Only a few of the studies on the treatment of dark spots on the hands mentioned above reported an improvement in photo-induced lines and wrinkles with specific creams(19–21). In 2018, Robati et al. achieved substantial clinical improvement in wrinkles on the skin of the back of the hands by laser therapy, without serious side-effects(31).
For skin laxity on the back of the knuckles, the author currently favours the mesolift therapy but other therapeutic solutions could also be considered. The data is still lacking in this area.
Unsightly veins visible under the skin are mainly treated by transcutaneous laser in the author’s office to make them less apparent. The objective is the same as that of light sclerotherapy, that is to say, reducing the diameter of the veins without destroying them.
Excess skin, bone deformations in the hands, and stripping require surgery. The new trend in cosmetic surgery is lipofilling for the hands or lipomodelling or an autograft of purified adipose tissue. This technique can rejuvenate the visible surface of the hand in a very natural way in one intervention with long-term results, while diminishing the appearance of veins and tendons32.
The author’s practice is limited to non-surgical aesthetic interventions. They do not perform surgical procedures and refer patients to specialised colleagues at their request.
The evaluation of the effectiveness of aesthetic interventions is based on the following criteria:
- Taking comparative digital photographs before and after the intervention as the reference
- Patient satisfaction with the care provided
- The evaluation of the physician by a clinical examination of the treated area(s)
- Clinical tolerance.
Analysing results
To date, no imaging tool exists to analyse the ageing process of the hand, yet advances in three-dimensional imaging provide complementary information for planning the diagnosis as well as evaluating the treatment outcomes.
Until now, the face is the most studied area for filler techniques(33).
A pilot study was conducted by Hoevenaren et al. to analyse the ageing process of the hand with three-dimensional stereophotogrammetry. This non-invasive 3D imaging technique offers the possibility to visualise the precise areas of volume loss of the dorsal surface of the hand, to identify the treatment areas and to evaluate the results obtained objectively and comparatively(34).
Further studies testing imaging techniques are needed to assess their role in daily practice.

At the end of this discussion, it is important to remember that over-the-counter devices are available for individuals, such as flash lamp systems, superficial glycolic acid peels, as well as depigmentation or whitening products available via the internet or in shops specialising in beauty products for black skin. All of these techniques can be ineffective or even the source of undesirable effects. Activity in this area is also widely practised by general practitioners, some of whom claim to be aesthetic physicians yet are untrained. When treatments are performed by a competent, trained physician, very few risks and dangers can occur.
Conclusion
Medico-aesthetic hand rejuvenation, without surgery, is now an integral part of the anti-ageing practice. Our current therapeutic arsenal is broad and offers satisfactory results. To date, there is no truly consensual protocol, since the treatment modalities vary according to the professional experience of each practitioner. Additional studies, which include a large sample of patients and have sufficient follow-up, are essential for the optimal therapeutic management of ageing hands, which can frequently betray the patient’s age. Therapeutic approaches, such as how to best combine treatments and the order in which treatment interventions would be most effective, remain to be studied in order to obtain optimal results that respond to the patients’ concerns.
Declaration of interest None
References
- Jakubietz RG, Kloss DF, Gruenert JG, Jakubietz MG. The ageing hand. A study to evaluate the chronological ageing process of the hand. J Plast Reconstr Aesthet Surg.2008 Jun;61(6):681-6
- Soleymani T, Lanoue J, Rahman Z. A Practical Approach to Chemical Peels: A Review of Fundamentals and Step-by-step Algorithmic Protocol for Treatment. J Clin Aesthet Dermatol.2018 Aug;11(8):21-28
- Deprez P. Textbook of Chemical Peel. Ed Dunitz Feb 2007:+/- 500pp.
- Cabotin PP. http://www.peaunoire.net/index.php/fiches-pratiques/laser-depigmentant
- Fusade T. Traitements lasers et peaux foncées. Réalités Thérapeut Dermatol Vénérol. Déc 2017;n°267-Cahier 1:35-36
- Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color.J Clin Aesthet Dermatol.2010 Jul;3(7):20-31
- Passeron T. L’hyperpigmentation post-inflammatoire. Ann. Dermatol. Venereol. 2016 déc; Vol.143, n°S2:15-19: S15-S19
- Brandt FS, Cazzaniga A, Strangman N, Coleman J, Axford-Gatley R. Long-term effectiveness and safety of small gel particle hyaluronic acid for hand rejuvenation. Dermatol Surg. 2012 Jul;38 (7 Pt 2):1128-35
- Dallara JM. A prospective, noninterventional study of the treatment of the ageing hand with Juvéderm Ultra® 3 and Juvéderm® Hydrate. Aesthetic Plast Surg. 2012:36(4):949-54
- Gubanova EI, Starovatova PA, Rodina MY. 12-month effects of stabilized hyaluronic acid gel compared with saline for rejuvenation of ageing hands. J Drugs Dermatol. 2015 Mar;14(3):288-98
- Khosravani N, Weber L, Patel R, Patel A. The 5-Step Filler Hand Rejuvenation: Filling with Hyaluronic Acid. Plast Reconstr Surg Glob Open.2019 Jan;7(1):e2073
- De Goursac C. Rajeunissement du visage et du corps par fils tenseurs résorbables. www.afme.org. Mars 2016
- De Goursac C. Les fils tenseurs résorbables en polydioxanone : une technique médico-esthétique pour “lifter les fessiers”. SFME J. Méd. Esth. et Chir. Derm. Déc 2018, Vol. XXXXV, 180:193-199
- Larrouy J-C. Traitement laser Nd:YAG Long Pulse des veines superficielles de la main. Recherche d’un aspect esthétique irréprochable. Ann. Dermatol. Venerol. Juin 2012; Vol.139,n 6-7S1:H71-H72
- Fanous N, Zari S. Universal Trichloroacetic Acid Peel Technique for Light and Dark Skin. JAMA Facial Plast Surg.2017;19(3):212-219
- Kung KY, Shek SY,Yeung CK, Chan HH. Evaluation of the safety and efficacy of the dual wavelength picosecond laser for the treatment of benign pigmented lesions in Asians. Lasers Surg Med.2019 Jan;51(1):14-22
- Friedmann DP, Peterson JD. Efficacy and safety of intense pulsed light with a KTP filter for the treatment of solar lentigines. Lasers Surg Med. 2019 Jan;51(1):14-22
- Schoenewolf NL, Hafner J, Dummer R, Bogdan Allemann I. Laser treatment of solar lentigines on dorsum of hands: QS Ruby laser versus ablative CO2 fractional laser – a randomized controlled trial. Eur J Dermatol.2015 Apr;25(2):122-6
- Roberts WE, Colvan L, Gotz V. Topical Treatment of Ageing Hands: Brief Report. J Clin Aesthet Dermatol. 2017 Aug; 10(8): 37-41
- Schlessinger J, Saxena S, Mohr S. Assessment of a novel anti-ageing hand cream. J Drugs Dermatol. 2016;15:496-503
- Gold MH, Gallagher C. An evaluation of the benefits of a topical treatment in the improvement of photodamaged hands with age spots, freckles, and/or discolorations. J Drug Dermatol.2013;12:1468-1472.
- Reinhold U, Hadshiew I, Melzer A, Prechtl. A.Low-dose 5-fluorouracil in combination with salicylic acid for the treatment of actinic keratoses on the hands and/or forearms – results of a non-interventional study. J Eur Acad Dermatol Venereol.2017; 31(3):455-462
- Uhlenhake EE. Optimal treatment of actinic keratoses. Clin Interv Ageing.2013;8:29-35
- Beylot C, Raimbault-Gerard. Les hyperpigmentations post-inflammatoires succédant à des actes esthétiques Ann Dermatol Vénéréol déc 2016 ;Vol 143, S2:33-42
- Todd MM, Rallis TM, Gerwels JW, Hata TR. A comparison of 3 lasers and liquid nitrogen in the treatment of solar lentigines: a randomized, controlled, comparative trial. Arch Dermatol.2000 Jul;136(7):841-6
- Rivkin AZ. Volume correction in the ageing hand: role of dermal fillers. Clin Cosmet Investig Dermatol.2016 Aug:225-32
- Kim JS. Detailed Sonographic Anatomy of Dorsal Hand Augmentation With Hyaluronic Acid and Calcium Hydroxyapatite Fillers. AesthetSurg J.2018 Sep 5
- Graivier MH, Lorenc ZP, Bass LM, Fitzgerald R, Goldberg DJ. Calcium Hydroxyapatite (CaHA) Indication for Hand Rejuvenation. Aesthet Surg J.2018 Apr 6;38(suppl-1):S24-S28
- Goldman MP, Moradi A, Gold MH, Friedmann DP, Alizadeh K, Adelglass JM, Katz BE. Calcium Hydroxylapatite Dermal Filler for Treatment of Dorsal Hand Volume Loss: Results From a 12-Month, Multicenter, Randomized, Blinded Trial. Dermatol Surg.2018 Jan;44(1):75-83
- Frank K, Koban K, Targosinski S, Erlbacher K, Schenck TL, Casabona G, Braz AV, Pavicic T, Cotofana S. The Anatomy behind Adverse Events in Hand Volumizing Procedures: Retrospective Evaluations of 11 Years of Experience. Plast ReconstrSurg.2018 May;141(5):650e-662e
- Robati RM, Asadi E, Shafiee A, Namazi N, Talebi A. Efficacy of long pulse Nd:YAG laser versus fractional Er:YAG laser in the treatment of hand wrinkles. Lasers Med Sci.2018 Apr;33(3):461-467
- Yun-Nan L, Shu-Hung H, Tsung-Ying L, Chih-Kang C, Yu-Hao H, Hidenobu T, Chung-Sheng L, Sin-Daw L, Tsai-Ming L. Micro-autologous fat transplantation for rejuvenation of the dorsal surface of the ageing hand. J Plast Reconstr Aesthet Surg.2018 Apr;71(4):573-584
- Goldman MP, Skover GR, Payonk GS. Three-dimensional imageing techniques in the assessment of facial volume augmentation. J Drugs Dermatol 2009;12:1113-9
- Hoevenaren IA, Wesselius TS, Meulstee JW, Maal TJ, Ulrich DJ. The effect of ageing on the three-dimensional aspect of the hand: A pilot study. J Plast Reconstr Aesthet Surg.2017 Apr;70(4):495-500.