
Firas Al-Niaimi, MSc, MRCP, EBDV, is a world renowned professor in dermatology and the only laser dermatology professor in the UK with a significant academic portfolio and over 220 scientific publications mostly in the laser field. He practices both in London and Denmark.
The Nd:YAG wavelength is a common wavelength used in dermatology, which is generated through the Neodymium-doped yttrium aluminium garnet crystal at a wavelength of 1064 nm in the near-infrared range of the electromagnetic spectrum. The Nd:YAG as a wavelength is uniquely positioned in terms of the absorption coefficients of the three main chromophores in the skin (water, melanin, and haemoglobin), and it is this advantage that makes the Nd:YAG laser popular as a treatment for multiple conditions that require targeting these chromophores1. The effects on the skin depend partly on the pulse duration, which can range from a millisecond down to the ultrashort pulse duration in the picosecond domain.
In this article, we discuss the uses of the long-pulsed Nd:YAG, which is in the microsecond and millisecond range. Hair removal will not be discussed, but it is worth noting that this wavelength is the main wavelength used in hair removal in darker skin types, given its preferential deeper penetration compared to the alexandrite laser and its relatively lower melanin absorption, which decreases the risk of epidermal injury2. In lighter skin types, the Nd:YAG can also be used in tanned individuals for similar reasons.
Vascular uses
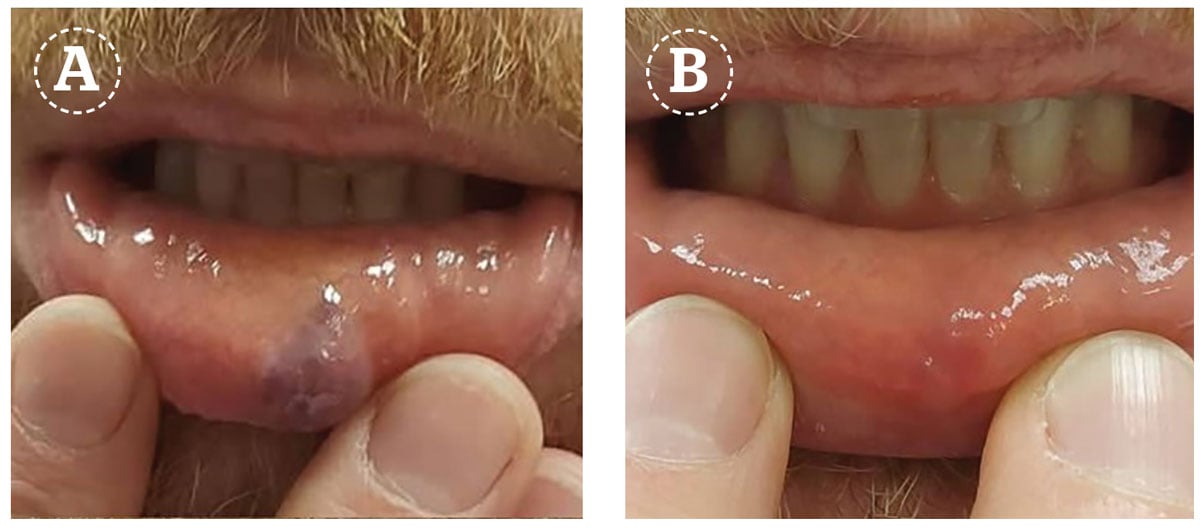
As mentioned in the introduction, the Nd:YAG wavelength is absorbed by haemoglobin which is why this laser can be used for a number of vascular conditions in dermatology. In particular, venous lesions respond preferentially to the Nd:YAG compared to the shorter vascular wavelengths (such as the 595 and 532 nm) as they are located deeper in the skin and are rich in deoxyhaemoglobin which is well absorbed by the Nd:YAG wavelength. The combination of these two characteristics makes this wavelength the first choice for venous lesions, such as leg veins, venules on the face and thick or hypertrophic parts of haemangiomas, and port-wine stains3.
Venules on the face respond well to the Nd:YAG and are safe to treat using a small spot and starting with low fluences, given the risk of atrophic scarring when a large spot size and high fluences are used. In one study comparing both the Nd:YAG laser against the pulsed dye laser (PDL) for nasal vessels, it was found that the small red telangiectasia responded better to the PDL, whereas the blue venules responded better to the Nd:YAG laser; an observation agreed with by laser experts4.
A study on the comparison between the Nd:YAG long-pulsed laser against the 532 nm vascular laser in leg vessels showed that the longer penetration of the Nd:YAG wavelength was superior to the 532 nm laser given the deeper uniform heating, which addressed the lower parts of the vessels since only the upper part of some vessels were in interaction with the shorter 532 nm wavelength5. The parameters of the Nd:YAG in leg vessels depend on the size and depth of the leg vessels, with typically smaller vessels requiring a smaller spot size and a shorter pulse duration and larger vessels requiring a slightly larger spot size (maximum 7 mm) and a longer pulse duration6. The clinical endpoint is important, which is colour change, spasm or disappearance of the vessel.
The gold standard treatment for port-wine stains remains the PDL, although there are reports of intense pulsed light (IPL) and 532 nm treatment in this condition. The hypertrophic component of port-wine stains responds less well to the shorter wavelengths and is preferentially treated with the Nd:YAG wavelength. The hypertrophic blebs and the purple colour of the vessels imply larger calibre vessels located deep in the skin hence their response to the Nd:YAG laser7. Indeed in a study among Chinese patients, it was demonstrated that for the purple component of the port-wine stain, the Nd:YAG was efficient, albeit it should be used with care and expertise8.
The treatment of haemangiomas has been transformed over the last decade since the discovery of the efficacy of systemic beta-blockers in this condition. Nevertheless, the Nd:YAG laser has been used in combination with the PDL in the treatment of the deeper component of the haemangiomas with success.
The author uses the Nd:YAG laser from both the Nordlys system (Candela Corporation, Marlborough, MA, USA) as well as the GentleMax Pro platform (Candela Corporation, Marlborough, MA, USA).
Scars
The use of lasers in the treatment of scars has been transformational over the last decade since it was found that fractional lasers remodel scar tissue and improve outcomes such as pliability, colour, and thickness. Vascular lasers play an integral part in laser scar therapy beyond just simply targeting the vascular component of the erythema. The Nd:YAG laser has been used in several studies in hypertrophic and keloid scars with demonstrable changes at a molecular level in the scar tissue, such as upregulating transforming growth factor beta 3 (TGF-b3) and reduction in collagen type 19. Treatment with the Nd:YAG should take into consideration the scar colour and thickness as well as the background skin type and is typically achieved with mid-spot sizes (4–7 mm) and fluences below the purpuric threshold. The use of microsecond pulse Nd:YAG has also been reported in scars, particularly in the treatment of atrophic scars.
An interesting finding in a study on keloids using the Nd:YAG laser is the benefit this wavelength has on the pain symptoms of a keloid10. The authors attribute this to the deep penetration of the wavelength which reaches the nerve plexus responsible for the pain sensation in some keloids. The use of the Nd:YAG laser in both hypertrophic and keloid scars is a subject of ongoing interest, with studies continuing to examine the utility of this wavelength in the field of scar management.
Warts
The Nd:YAG laser is very effective in the treatment of cutaneous warts and verrucae, and its use in this cutaneous infection has been published in several series, including among higher Fitzpatrick scale skin types in a study from Korea11. One limitation of the treatment could be the relatively high pain sensation this treatment is associated with, but it has been demonstrated to clear cutaneous warts effectively, at times with as little as a single treatment session12. Typical parameters would be a small spot size and a pulse duration of between 20 to 30 ms, and relatively high fluences13. It is thought that the mechanism of action is a combination of papillary vessel coagulation or necrosis together with clefting of the dermo-epidermal junction as a result of the thermal effect, a mechanism explaining the need for relatively high fluences. Overall the recurrence rate seems to be relatively low in this method of treatment, and therefore the Nd:YAG could be an excellent choice of treatment, particularly for resistant or multiple warts unresponsive to topical therapy.
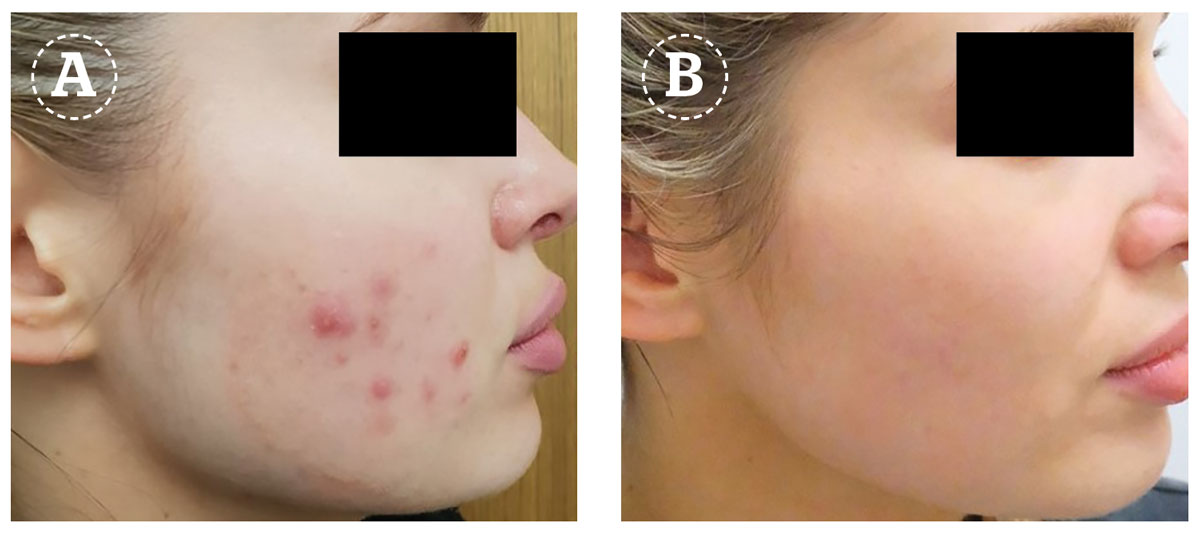
Acne
Acne vulgaris is a common inflammatory skin condition of the pilosebaceous unit. While there are established medical therapies in terms of topical and systemic therapy for this condition, patients with milder forms of acne are increasingly seeking laser treatment given their reluctance for medical therapy14. The Nd:YAG laser has been used in acne for many years, with several studies published on its efficacy in the mild to moderate forms of acne. Both the pulsed millisecond as well as the painting technique with the microsecond pulses have been used15,16. The mechanism involves thermal effects on the sebaceous glands with a degree of microvessel coagulation and the generation of heat shock proteins that recreate a bactericidal effect against the c.acnes bacteria. Combination treatment with other established acne therapies may lead to faster response and synergism in response to treatment.
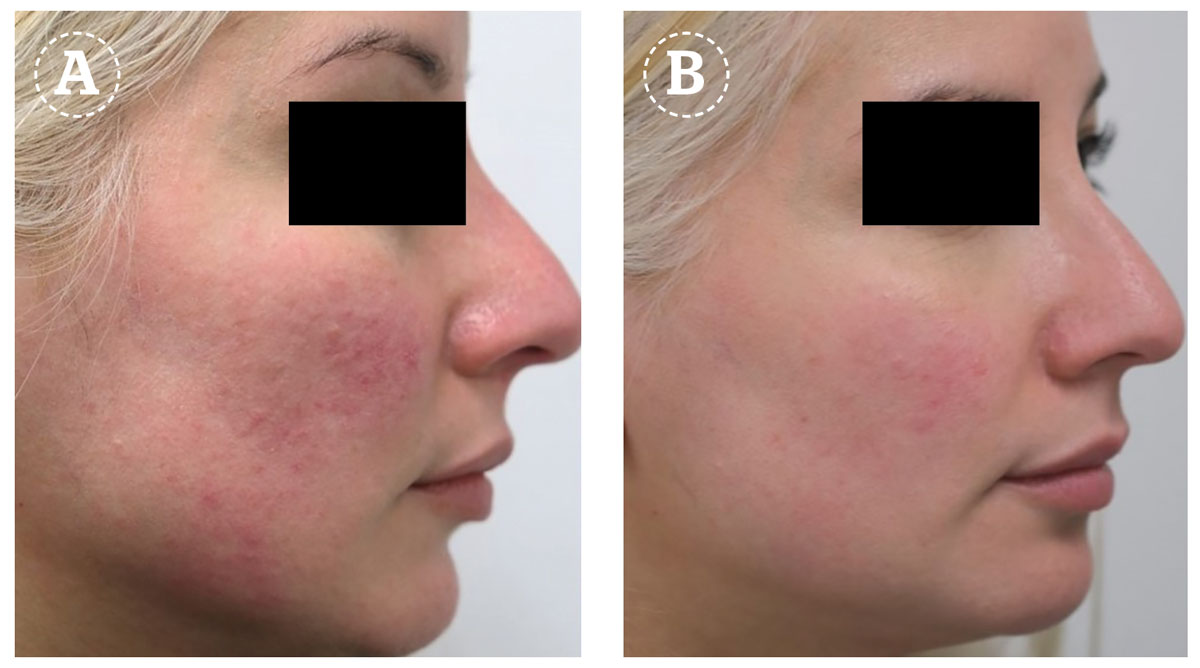
Rosacea/diffuse redness
Papulopustular acne, as well as diffuse redness and vascular rosacea, have been successfully treated with the Nd:YAG laser in both the millisecond pulsed mode as well as the painting mode with the microsecond pulse17. As discussed earlier, the Nd:YAG wavelength is absorbed by haemoglobin hence its efficacy in diffuse redness due to the photothermal effects leading to vessel coagulation. Particularly the short pulse duration would be more suitable for the treatment of diffuse redness since the small vessel size would have a short thermal relaxation time. In one study among patients with papulopustular rosacea, the use of long-pulsed Nd:YAG led to good clearance of the majority of patients with no complications18,19. In practice, the Nd:YAG laser can be combined with other topical or systemic therapies for rosacea for a synergistic effect.
Onychomycosis
Fungal nail infection is a common problem worldwide, and while there are systemic treatments for this condition, the use of lasers might be an alternative for patients who are unable to or unwilling to take systemic treatment in the form of tablets. The Nd:YAG has been reported in numerous studies to be effective in onychomycosis, with typically several treatments needed at around monthly intervals20. There is some variation in terms of parameters — in particular, the pulse duration — but it is generally the short pulse durations in the nano and microsecond range that tend to be effective21,22. The author prefers to use the microsecond pulse duration with a high repetition rate, with heat generation being the suggested mechanism behind its efficacy.
Hair follicle-related disorders
In addition to laser treatment of hirsutism or unwanted hair for aesthetic reasons, the Nd:YAG laser has been used in a number of follicle-related disorders with or without combination treatment with favourable outcomes. These conditions include hidradenitis suppurativa, pilonidal sinus (particularly post-surgery), dissecting cellulitis, keratosis pilaris, and pseudofolliculitis barbae23.
Rejuvenation
The Nd:YAG laser, as mentioned previously, is a wavelength that is absorbed by all three main skin chromophores: haemoglobin, melanin, and water. The absorption by water is particularly enhanced in the short microsecond wavelength where there is little to no melanin and haemoglobin absorption, and with a high repetition rate there can be a build-up of heat in the skin that may eventually with repeated treatments lead to rejuvenation with texture improvement, pore tightening, and some tissue firming and rejuvenation24. In some reports, the procedure uses long pulsed Nd:YAG in the millisecond range25.
Conclusion
The Nd:YAG is a near-infrared wavelength that has the unique position of being absorbed by all three main skin chromophores: haemoglobin, water, and melanin. It has, therefore, multiple uses in dermatology, from vascular to hair removal and numerous other conditions such as scars, acne, and warts, to name just a few. The treatments can be combined with other modalities and may, in some cases, require several sessions. The Nd:YAG plays an important role in the field of laser dermatology, and ongoing interest in its uses are still being explored.
- Declaration of interest Funding for submission of this paper was provided by Candela
- Figures 1-3 © Candela Corporation
References
- Gan SD, Graber EM. Laser hair removal: a review. Dermatol Surg. 2013 Jun;39(6):823-38.
-
Kaur Hora M, Choudhary N, Agrawal S, Gupta S, Gandhi J, De A, Chatterjee G. Evaluation of the Efficacy and Safety Profile of Long-Pulsed 1064 Neodymium:Yttrium-Aluminum-Garnet (Nd:YAG) Laser in Hemangioma and Vascular Malformation in Darker Skin Types. Cureus. 2022 Jun 8;14(6):e25742.
-
Bäumler W, Ulrich H, Hartl A, Landthaler M, Shafirstein G. Optimal parameters for the treatment of leg veins using Nd:YAG lasers at 1064 nm. Br J Dermatol. 2006 Aug;155(2):364-71.
-
Adamic M, Troilius A, Adatto M, Drosner M, Dahmane R. Vascular lasers and IPLS: guidelines for care from the European Society for Laser Dermatology (ESLD). J Cosmet Laser Ther. 2007 Jun;9(2):113-24.
-
Akaishi S, Koike S, Dohi T, Kobe K, Hyakusoku H, Ogawa R. Nd:YAG Laser Treatment of Keloids and Hypertrophic Scars. Eplasty. 2012;12:e1. Epub 2012 Jan 11.
-
Shrestha S , Karn D . Long Pulsed Nd:YAG Lasers in the Management of Cutaneous Warts. Kathmandu Univ Med J (KUMJ). 2018 Jan.-Mar;16(61):60-64.
-
Le HTT, Truong Van C, Nguyen Thi M, Al-Niaimi F. Our experience using 1064 nm Nd:YAG in palmoplantar warts. J Cosmet Laser Ther. 2022 Jul 4;24(1-5):28-32.
-
Han TY, Lee JH, Lee CK, Ahn JY, Seo SJ, Hong CK. Long-pulsed Nd:YAG laser treatment of warts: report on a series of 369 cases. J Korean Med Sci. 2009 Oct;24(5):889-93.
-
Li MK, Liu C, Hsu JTS. The Use of Lasers and Light Devices in Acne Management: An Update. Am J Clin Dermatol. 2021 Nov;22(6):785-800.
-
Chalermsuwiwattanakan N, Rojhirunsakool S, Kamanamool N, Kanokrungsee S, Udompataikul M. The comparative study of efficacy between 1064-nm long-pulsed Nd:YAG laser and 595-nm pulsed dye laser for the treatment of acne vulgaris. J Cosmet Dermatol. 2021 Jul;20(7):2108-2115.
-
Ballin JS, Uebelhoer NS. The use of the low-fluence 1064 nm Nd:YAG laser in a female with contraindications to systemic anti-acne therapy. J Drugs Dermatol. 2009 Nov;8(11):1025-6.
-
Alam M, Voravutinon N, Warycha M, Whiting D, Nodzenski M, Yoo S, West DP, Veledar E, Poon E. Comparative effectiveness of nonpurpuragenic 595-nm pulsed dye laser and microsecond 1064-nm neodymium:yttrium-aluminum-garnet laser for treatment of diffuse facial erythema: A double-blind randomized controlled trial. J Am Acad Dermatol. 2013 Sep;69(3):438-43.
-
Salem SA, Abdel Fattah NS, Tantawy SM, El-Badawy NM, Abd El-Aziz YA. Neodymium-yttrium aluminum garnet laser versus pulsed dye laser in erythemato-telangiectatic rosacea: comparison of clinical efficacy and effect on cutaneous substance (P) expression. J Cosmet Dermatol. 2013 Sep;12(3):187-94.
-
Kwon WJ, Park BW, Cho EB, Park EJ, Kim KH, Kim KJ. Comparison of efficacy between long-pulsed Nd:YAG laser and pulsed dye laser to treat rosacea-associated nasal telangiectasia. J Cosmet Laser Ther. 2018 Oct;20(5):260-264.
-
Say EM, Okan G, Gökdemir G. Treatment Outcomes of Long-Pulsed Nd: YAG Laser for Two Different Subtypes of Rosacea. J Clin Aesthet Dermatol. 2015 Sep;8(9):16-20.
-
Ma W, Si C, Kasyanju Carrero LM, Liu HF, Yin XF, Liu J, Xu Y, Zhou B. Laser treatment for onychomycosis: A systematic review and meta-analysis. Medicine (Baltimore). 2019 Nov;98(48):e17948.
-
Kim MS, Jung JY, Cho EB, Park EJ, Kim KH, Kim KJ. The effectiveness of 1,064-nm long-pulsed Nd:YAG laser in the treatment of severe onychomycosis. J Cosmet Laser Ther. 2016 Oct;18(6):317-22.
-
Okan G, Tarikci N, Gokdemir G. The Effect of Long-Pulsed Nd:YAG Laser for the Treatment of Onychomycosis. J Am Podiatr Med Assoc. 2017 Jan;107(1):54-59.
-
Chiba C, Usui A, Hara H, Ishi Y. Clinical experience in skin rejuvenation treatment in Asians using a long-pulse Nd:YAG laser. J Cosmet Laser Ther. 2009 Sep;11(3):134-
-
Kaya TI, Guvenc U. Long pulse 1,064-nm neodymium-doped yttrium aluminum garnet laser in aesthetic dermatology. Dermatol Ther. 2019 May;32(3):e12907.
-
Hong JS, Park SY, Seo KK, Goo BL, Hwang EJ, Park GY, Eun HC. Long pulsed 1064 nm Nd:YAG laser treatment for wrinkle reduction and skin laxity: evaluation of new parameters. Int J Dermatol. 2015 Sep;54(9):e345-50.
-
Chiba C, Usui A, Hara H, Ishi Y. Clinical experience in skin rejuvenation treatment in Asians using a long-pulse Nd:YAG laser. J Cosmet Laser Ther. 2009 Sep;11(3):134-8.






