ABSTRACT
A typical concept in aesthetic dermatology is the controlled stimulation of epidermal and dermal structures for skin rejuvenation. Multiple modalities are available, among which platelet-rich plasma (PRP) plays a role. PRP injection is a therapeutic approach using the tools of biologic regeneration of the autologous cells and tissues rather than their replacement. For a reliable and aesthetically-appealing outcome of PRP injections for skin rejuvenation, it is paramount to highlight the differences in preparation, composition, and handling of PRP, as well as the clinical proof of its action. The further we go in using and administering autologous PRP, the more we will understand how important high quality features and the proof of the clinical mode of action are for effective, aesthetically-appealing, and safe skin rejuvenation.
Ageing is a highly individualised phenomenon, from person-to-person, and regardless of gender, origin, and lifestyle, ‘each patient looks old for their own reasons and in their own way’1. Despite this, the processes involved in ageing in the dermal layers will not vary. Using confocal laser scan microscopy (CLSM), it is possible to see that in the upper dermis of young skin, collagen fibres appear as bright, elongated fibrillar structures, which form a web-like structure. However, in aged skin, we can see that the collagen fibres have become curled and fragmented (Figure 1).
There are a variety of techniques available to replenish lost collagen and elastin, including the use of dermal fillers based on hyaluronic acid and calcium hydroxylapatite formulations. Autologous platelet-rich plasma (PRP) has also been found to play an important role in tissue healing and rejuvenation, and has been used for a variety of indications for more than 30 years2, being well-documented in the fields of dentistry, maxillofacial surgery, and orthopaedics3–6. Since 2005, PRP has also begun to be used for aesthetic indications, as it has been found to possess growth-promoting properties to accelerate the repair of aged and damaged soft tissues7,8. It achieves this by stimulating a thickening of the superficial layer of the skin and collagen remodeling, improving cell regeneration and blood supply to the specific tissue.
Indeed, in aesthetic medicine, PRP is indicated for superficial dermal stimulation and dermal augmentation.
Preparation and injection techniques
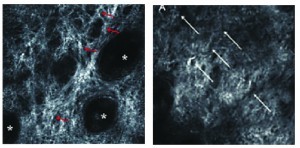
Figure 1 (A) The upper dermis in young skin—collagen fibres appear as bright, elongated fibrillar structures forming a web, and (B) the upper dermis in aged skin, fibres appear curled, and fragmented.
PRP is derived from a patient’s whole blood and processed in a centrifuge, which removes the red blood cells and leaves a high concentration of platelets and growth factors. The PRP can then be activated with thrombin or calcium chloride. This activation causes the platelets to begin releasing growth factors, but the PRP can also be injected in its inactivated form, allowing it to be activated once it is within the injection site. It is estimated that after centrifugation, there is a two-fold increase in platelet concentration above baseline in venous blood9.
PRP contains a number of growth factors, hormones, nutrients, protein stabilisers (e.g. albumin), and other important bioactive compounds for cellular growth and homeostasis10. The aim of treatment with PRP is to maximise the growth factors found in alpha-granules to promote an anabolic environment at the site of injection.
The mechanism of action of PRP is only partly understood. A number of different growth factors are known to be released by the platelets11–13, including:
- Platelet-derived growth factor (PDGF) has its main origin in the platelets and impacts on the proliferation and chemotaxis of fibroblasts, effects mitogenesis of the mesenchymal stem cells and endothelial cells, and promotes the synthesis of the extracellular matrix and hyaluronan production
- Transforming growth factors α and β (TGF-α, -β) also have their origin in the platelets and promote cell mitosis (fibroblasts), collagen production, stimulation of DNA synthesis, expression of antimicrobial peptides, keratinocyte stimulation, and angiogenesis
- Vascular endothelial growth factor (VEGF) stimulates angiogenesis and endothelial cell proliferation
- Epidermal growth factor (EGF) regulates cell growth, stimulates the proliferation and differentiation of the epidermic cells, promotes granulation tissue formation, and co-stimulates angiogenesis
- Fibroblast growth factor (FGF-1, -2) stimulates fibroblast chemotaxis, angiogenesis, matrix (collagen fibre) deposition, and wound contraction.
The activated platelets will synthesise and release these growth factors over the next 7–10 days once the cascade has begun12.
The combination of calcium chloride and PRP in a defined stoichiometric ratio results in the initiation of fibrin polymerisation , while leaving the platelets intact14–17. This, in turn, leads to the formation of a platelet-rich fibrin matrix (PRFM). PRFM is a term used for PRP, which once activated, leads to fibrin polymerisation, and builds the scaffold for the thrombocytes to enable a sustained growth factor release.
PRP is used in the aesthetic field for the stimulation of the dermis. Most scientific proof for PRP as a stand-alone therapy can be found for the mesotherapy-type injection for skin rejuvenation: the injection itself is either performed using a multipuncture or a micropapular technique. Some authors appreciate the inter- or subdermal injection to perform stimulation, but there is a lack of scientific proof for these techniques.




