Anastasia Mashkina describes her treatment regimens for the range of complications that can arise following botulinum toxin injections

Dermatologist, cosmetologist, international expert in rejuvenation injection techniques, Moscow, Russia
email: [email protected]
The emergence of botulinum toxins in cosmetology many years ago was a real revolution. Ever since, injections of botulinum toxins have become one of the most popular procedures all over the world. Their number is continually growing; the availability of the procedure is increasing, and consequently, as is the number of consumers. However, at the same time, the number of complications resulting from botulinum toxin injections is also on the rise.
Treatment complications are undoubtedly one of the least pleasant sides of the profession. However, every doctor, at least once during their time in practice, is presented with undesirable results. We must be confident we are able to treat these complications when they arise and help our patients.
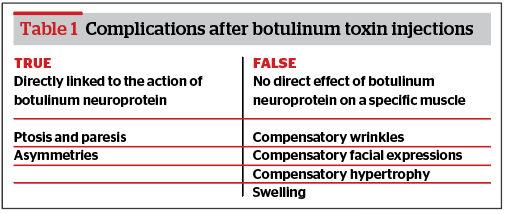
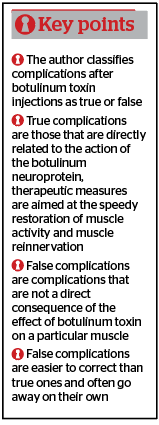
My thoughts on complications after botulinum toxin injections are based on 10 years of experience working with toxins, as well as on the practical aspects of their treatment. I classify complications after botulinum toxin injections as either true or false (Table 1).
True complications
True complications are those that are directly related to the action of the botulinum neuroprotein:
Ptosis and paresis — complications resulting from strong muscle relaxation as a result of the direct action of a large dose of botulinum toxin on the muscle (eyelid ptosis, eyebrow drooping, impaired articulation, fluid pouring from the corner of the mouth).
Asymmetries — complications associated with a transgression to the injection technique, incorrect placement and level of botulinum toxin injection, incorrect dose, or the diffusion of botulinum toxin into adjacent muscles. This can present as eyebrow asymmetry, asymmetry of the mouth, asymmetry when opening the mouth, tightening the lips, changing the shape of the chin).
Ptosis and paresis cannot be corrected by additional injections of botulinum toxin. Therapeutic measures are aimed at the speedy restoration of muscle activity and muscle reinnervation.
Scheme 1
- Scheme 1 deals with the treatment of excessive muscle relaxation after botulinum toxin injections.
- The following are the recommended treatment protocols when addressing excessive muscle relaxation.
- PRP therapy — 3 times a week
- B vitamins orally for 2 weeks and mesotherapy treatment of the lesion site once every 2 days
- Mesotherapy with DMAE solution — twice weekly using the micro papule technique
- Microcurrent therapy (3–5 times a week), myostimulation (1–2 times a week), RF therapy once a week. These procedures can be independent or prescribed in a complex. The total number of physiotherapy procedures should not exceed five per week. For example, one RF therapy procedure, one myostimulation procedure, three microcurrent therapy procedures.
- Pinch massage of the complication zone — daily
- Mimic gymnastics — 3 times a day for 15 minutes, daily
- Placental preparations, one ampoule two times a week at bioactive points or intramuscularly in the complication zone.

For upper eyelid ptosis, eye drops of 0.5% Apraclonidine have a temporary effect. The drug is an agonist of alpha-2-adrenergic receptors of smooth muscles and, when it enters the eyeball, causes the contraction of the Müller’s muscle, which contributes to raising the upper eyelid by 2–3 mm for several hours. The author would recommend inserting 1–2 drops three times a day.
To activate the restoration of neuromuscular transmission, the author prescribes Ipidacrinum 10 mg, one tablet to be taken orally, two times a day for 14 days.
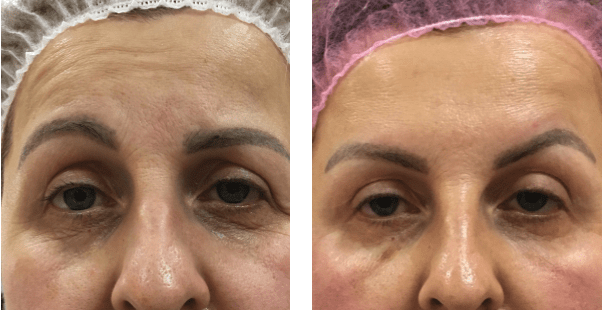
Upper eyelid ptosis
Patient 1 complained of upper eyelid ptosis 2 weeks after injections of botulinum toxin in the glabella region with a total dose of 10 U (100 U toxin). Ptosis of the eyelid presented on the 7th day after the injection. Over the next week, ptosis progressed (Figure 1). From the 14th day, for 2 weeks, the patient received therapy according to scheme 1. In such cases, improvement in the condition can be observed within 2–6 weeks. The healing time is determined by the regenerative potential of the m.levator palpebrae superioris and the dose of diffused botulinum toxin: the stronger the muscle blockage, the longer the ptosis of the upper eyelid will be observed.

Unlike upper eyelid ptosis, eyebrow ptosis presents as the skin fold overhanging in the upper eyelid immobile part, while the drooping of the mobile eyelid is not observed. This complication is due to excessive relaxation of the m.frontalis, especially its lower part. In this case, restorative therapy should be carried out on the half of the forehead where the complication arose.
Eyebrow ptosis
Patient 2 complained of a skin fold overhanging in the right eyelid area 3 weeks after injections of botulinum toxin into the forehead and glabella region (Figure 2). When the patient tried to raise her eyebrows, we saw a strong frontal muscle relaxation. Unlike ptosis of the upper eyelid, ptosis of the eyebrows does not seem to be such a formidable problem. M. frontalis recovery can take 2 to 4 weeks. The patient noted an improvement in her condition 1 week after the start of therapy according to scheme 1.
Asymmetries in most cases are corrected by additional administrations of botulinum toxin. I use small doses of botulinum toxin intradermally to avoid reversing the asymmetry.
Eyebrow asymmetry
Patient 3 presented with a pronounced natural asymmetry around the eyebrows. The patient’s left eyebrow is lowered, while the right eyebrow is raised unnaturally. This aesthetic disadvantage can be compensated for by injecting different doses of botulinum toxin into symmetrical areas of the face. Two weeks after the injection of botulinum toxin in different doses into the glabella region and m.frontalis, the asymmetry reversed — the patient’s right eyebrow acquired a normal position, and the left eyebrow is now raised unnaturally (Figure 3). This complication can be easily corrected with the introduction of a small additional dose of botulinum toxin over the left eyebrow in the place of its maximum rise (2–2.5 U of 500 U toxins intradermally).
Frequent complications occur when correcting a bumpy chin. To mask such an aesthetic defect, injections of botulinum toxin into the m.mentalis are used. When relaxing the m.mentalis, it is very important to follow the correct injection technique. The numerous complications of a spade-shaped chin after such injections confirm the importance of maintaining the depth of the injections. This complication is associated with a violation of the injection depth and uneven blocking of the m.mentalis. In the lower sections, this muscle is deeply corrected, but in the upper sections, injections should be carried out superficially. The total dose for relaxation of the chin muscle is 6–8 units of 500 units of botulinum toxin.
Asymmetry of the lips

Figure 4 The result of diffusion of botulinum toxin into the m.depressor labii inferioris.
Patient 4 (Figure 4) 9 days after injections of botulinum toxin into the m.depressor anguli oris in order to raise the lips, the patient began to notice asymmetry when opening their mouth. In this situation, botulinum toxin was injected to a greater depth than necessary, as a result of which the fibres located deeper in the m.depressor labii inferioris were blocked, which led to its relaxation and an uneven rise of the lip on the left. Diffusion of botulinum toxin in the m.depressor labii inferioris occurred on the patient’s left side, which led to a rise in the left side of the lower lip and pronounced asymmetry in the smile. This complication quickly goes away on its own and is rarely corrected. The latter can be aimed either at restoring the innervation of the m.depressor labii inferioris on the diseased side according to scheme 1, or at light deinnervation of the same muscle on the healthy side with a mesotherapeutic concentration of botulinum toxin. In the second case, partial blocking of the muscle on the healthy side will compensatory ‘force’ the muscle of the diseased side to work faster, this will slightly correct the asymmetry. However, in the case of a doctor’s decision to correct botulinum toxin, injections must be performed at a strictly defined level, which requires a deep knowledge of the anatomy and location of the muscles.
False complications
- False complications are complications that are not a direct consequence of the effect of botulinum toxin on a particular muscle. The author refers to the so-called ‘compensatory manifestation’:
- Puffiness — when mimic muscles contract, they ‘push’ fluid from the tissues into the lymphatic capillaries, thereby improving lymph drainage. Excessive muscle relaxation leads to a deterioration in lymph flow
- Compensatory facial expressions — associated with the blockage of certain muscle groups and the appearance of facial activity in other areas where it was not previously
- Compensatory wrinkles — associated with the redistribution of tone in a particular muscle
- Compensatory hypertrophy — associated with muscle relaxation, in which friendly muscles begin to hypertrophy, assuming the function of blocked ones.
- False complications are easier to correct than true ones and often go away on their own. All ‘compensatory manifestations’ can be successfully corrected by additional administration of botulinum toxin, but it is more reasonable to foresee their appearance during the main procedure by performing prophylactic injections.
Swelling
An unpleasant complication after injections of botulinum toxin using the full face technique or into the m. orbicalaris oculi may cause swelling of the face, or only the malar bags or the area around the eyes. Usually, puffiness as a complication develops 7–8 days after botulinum toxin injections and can be present for an extended time until muscle activity is restored. To eliminate puffiness, we recommend using therapy according to scheme 2.
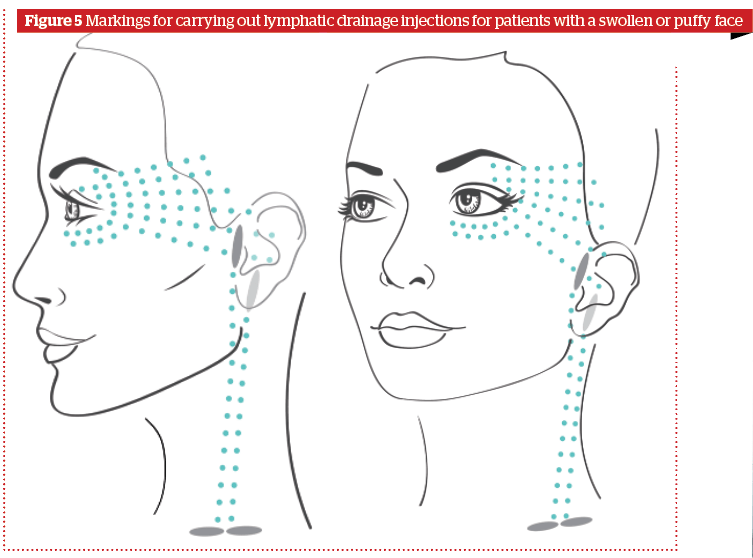
Scheme 2
The steps involved are as follows:
- Decongestant therapy for swollen or puffy appearance after injections of botulinum toxin
- Injections of drugs with a lymphatic drainage effect, according to a particular points (Figure 5). The marking is carried out in accordance with the location of the lymphatic vessels and lymph nodes. Lymphatic drainage cocktails can be used, combined drugs with sodium succinate, peptide drugs, and rutin-melilot
- A diet with no salt and alcohol
- Microcurrent therapy — daily
- Lymphatic drainage massage — daily.

Figure 6 Compensatory facial expressions after injections in m.orbicularis oculi.
Compensatory facial expressions
Patient 5 (Figure 6) was injected in the m.orbicularis oculi (Figure 6a shows mimic activity before injections). Seven days after the injection, wrinkles in the nasal area began to appear when smiling, although previously such mimic activity was not observed (Figure 6b). Correction involves injections of botulinum toxin into the m.nasalis.
Compensatory wrinkles
Patient 6 presented with small wrinkles above the eyebrows that formed 6 days after botulinum toxin injections in the m.frontalis and glabella region. Correction requires intradermal injection of botulinum toxin in a dose of 1–1.5 U (500 U) per injection. It is necessary to wait 2–3 weeks after the primary procedure before correction.

Figure 7 Compensatory wrinkles after botulinum toxin injections.
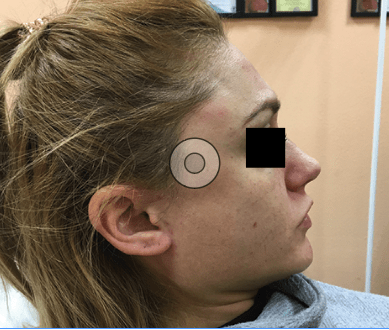
Compensatory hypertrophy
Patient seven’s temporal muscles significantly increased 12 days after botulinum toxin injections into both m. masseter muscles. Prophylactic injections into m. temporalis were not performed. The temporal muscles sharply outlined and increased. The patient needs additional injections of botulinum toxin into the temporal muscles.
Conclusion
It can be concluded that there are many complications after botulinum toxin injections and they are varied. However, the continuous improvement of knowledge in the field of anatomy, physiology, and pharmacokinetics of botulinum toxin gives us the strength and ability to use this unique remedy, which in the hands of a true professional is able to work wonders.
Declaration of interest None
Figures 1 © Dr Shadoba Olga; 2,3,6,8 © Dr Anastasia Mashkina; 4 © Dr. Dzerassa Mildzikhova; 7 © Dr. Alephtina Boyko
Table 1 © Dr Anastasia Mashkina
Further Reading
- Lowe P, Patnaik R, Lowe N. Comparison of two formulations of botulinum toxin type A for the treatment of glabellar lines: a double-blind, randomized study. J Am Acad Dermatol 2006;55:975–80.
- Frevert J, Dressler D. Complexing proteins in botulinum toxin type A drugs: a help or a hindrance? Biologics 2010;4:325–32.
- Lietzow MA, Gielow ET, Le D, Zhang J, et al. Subunit stoichiometry of the Clostridium botulinum type A neurotoxin complex determined using denaturing capillary electrophoresis. Protein J 2008;27:420–5.
- Brin MF, James C, Maltman J. Botulinum toxin type A products are not interchangeable: a review of the evidence. Biologics 2014;8:227–41.
- Abbasi NR, Durfee MA, Petrell K, Dover JS, et al. A small study of the relationship between abobotulinum toxin A concentration and forehead wrinkle reduction. Arch Dermatol 2012;148:119–21.
- Jost WH, Benecke R, Hauschke D, Jankovic J, et al. Clinical and pharmacological properties of incobotulinumtoxinA and its use in neurological disorders. Drug Des Devel Ther 2015;9:1913–26.
- Allen SB, Goldenberg NA. Pain difference associated with injection of abobotulinumtoxinA reconstituted with preserved saline and preservative-free saline: a prospective, randomized, side-by-side, double-blind study. Dermatol Surg 2012;38:867–70.
- Gracies JM, Lugassy M, Weisz DJ, Vecchio M, et al. Botulinum toxin dilution and endplate targeting in spasticity: a double-blind controlled study. Arch Phys Med Rehabil 2009;90:9–16.e2.
- Wei J, Xu H, Dong J, Li Q, et al. Prolonging the duration of masseter muscle reduction by adjusting the masticatory movements after the treatment of masseter muscle hypertrophy with botulinum toxin type a injection. Dermatol Surg 2015;41(Suppl 1):S101–9.
- Cliff SH, Judodihardjo H, Eltringham E. Different formulations of botulinum toxin type A have different migration characteristics: a double-blind, randomized study. J Cosmet Dermatol 2008;7:50–4.
- Lowe NJ, Shah A, Lowe PL, Patnaik R. Dosing, efficacy and safety plus the use of computerized photography for botulinum toxins type A for upper facial lines. J Cosmet Laser Ther 2010;12:106–11.
- Johnson EA, Bradshaw M. Clostridium botulinum and its neurotoxins: a metabolic and cellular perspective. Toxicon 2001;39:1703–22.







