Acne vulgaris is a common condition which remains challenging to treat in some cases. Laser and light-based therapies offer an alternative to medical therapies with the advantage of high compliance and relatively low side-effect profile. Light-based therapies in acne exert their effects through photochemical, photothermal, or a combination of both mechanisms. This article explains the mode of action for each light-based modality and examines the current evidence in this field.
Acne vulgaris is one of the most prevalent skin disorders, and often occurs in a large number of individuals during their adolescent years. It has the potential to cause significant scarring and psychological impact1. There are a large number of treatment options available to patients at present; however, these are not without side-effects and in many cases the disease can be resistant to therapy, hence the desire for additional, alternative treatment options. Non-compliance, the lack of desire for systemic therapy, coupled with the desire for the use of modern technology has led to an increase in the demand for alternative non-medical therapies in acne. Of late, interest in lasers and other light-based treatments has increased. One of the main advantages of the use of lasers in acne is the high degree of compliance and the negligible rate of potential systemic adverse events.
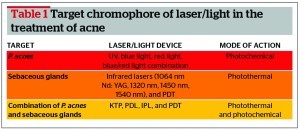
The mechanisms of light-based therapies in acne could be divided into photochemical effects (with or without the use of exogenous photosensitiser), photothermal effects, or the combination of both (Table 1). An alternative approach is to divide the effects of light-based therapies on specific targets in the skin, namely the Propionibacterium acnes (P. acnes), the follicular infundibulum, or the sebaceous glands. It is worth mentioning here that therapies directed at either of these targets will have a degree of anti-inflammatory effects, leading to an overall improvement in the treatment of acne.
Ultraviolet (UV) phototherapy is not often used in the treatment of acne owing to the carcinogenic potential and its mechanism of action is likely to be related to the production of superoxide anions, as well as membrane damage and single strand breaks in DNA2. Desquamative effects are also likely to play a role as well as a mild photochemical effect on the superficially-located P. acnes. Both visible and UV light sources have been reported to result in a reduced number of lesion counts3. Endogenous porphyrins within P. acnes are thought to absorb light at specific wavelengths which then produce phototoxic effects in the form of singlet oxygen production resulting in bacterial destruction4. Current hypothesis regarding infrared lasers is that they are thought to momentarily damage sebaceous glands via thermal effects5. This article explains the effectiveness of laser and light therapy in the treatment of acne. The article does not cover the treatment of acne scarring with laser and light devices.
Blue and red light
Low-level continuous light in the form of continuous, non-coherent blue and/or red light-emitting diodes (LEDs) were known to be used in acne for their photochemical effects. With pulsed systems, low fluences can exhibit similar photochemical effects depending on the tissue oxygen availability and may require an extrinsic photosensitiser or multiple passes in comparison to the continuous-output LEDs. Although blue light has poor skin penetration (less than 100- µm), with a wavelength of 407–420- nm it exhibits the strongest porphyrin photo-excitation co-efficient and is, therefore, the most effective wavelength to photoactivate the endogenous porphyrins contained in P. acnes6. The coproporphyrins, the main porphyrin produced by the P. acnes acts here as a chromophore. An in vitro study demonstrated that blue light activation of porphyrin led to structural membrane damage in P. acnes, suggesting cell death. Culture growths were indeed decreased 24 hours after one illumination with intense blue light at 407–420 nm. Growth was reduced 4–5 orders of magnitude further with second and third illuminations of light7.
One of the main limitations of blue light is its poor penetration and a degree of loss secondary to scattering or melanin absorption and its main target is therefore likely to be in the follicular infundibulum.
However, red light penetrates the skin at a deeper level, up to the sebaceous gland and is thought to have anti-inflammatory properties by influencing the release of cytokines from macrophages as well as photothermal effects directly aimed at the sebaceous glands8. There have been a number of studies involving both blue and/or red light in the treatment of acne. Most were open-labelled with few split-face comparative studies. The sample sizes were relatively small (20–50 patients) and all studies noted an improvement in acne lesions9.
One study looked at red light alone; when used in a split-faced randomised controlled trial there was a significant improvement in both inflammatory and non-inflammatory lesions9.
Five open label studies used the combination of blue and red light in 170 patients who were followed-up for a period of 2 to 3 months. In four of these studies, inflammatory lesions showed greater improvement than non-inflammatory lesions.
In summary, blue and red light may act synergistically in the treatment of acne through bactericidial effects (blue light) and anti-inflammatory effects (red light).
Pulse dye laser
The 585/595 nm pulse dye laser (PDL) targets oxyhaemaglobin and results in selective photothermolysis of the dilated vessels that form a part of the inflammatory process in inflammatory acne4. Possible additional mechanisms include a photochemical effect on the porphyrins produced by the P. acnes. Porphyrins are activated via the delivery of yellow light, which results in phototoxic effects4,6.
[pull_quote align=”left” ]One of the main advantages of the use of lasers in acne is the high degree of compliance and the negligible rate of potential systemic adverse events.[/pull_quote]
Fourteen studies using PDL to treat acneiform lesions have been reported in the literature. There were significant methodological differences between the studies; six studies used PDL therapy alone and five studies used PDL therapy combined with topical agents (5-aminolevulinic acid, methylaminolevulinic acid, clindamycin, or benzyl peroxide).
In the studies that used PDL in combination with topical agents, four cases reported an improvement in inflammatory lesions ranging from 30–80%. In cases of PDL used alone, three cases reported a significant reduction (53–86%) in inflammatory lesions. PDL did not significantly reduce the number of non-inflammatory lesions in any of the cases. Three studies reported PDL to have no significant change in the number of lesions when used alone or in combination with topical agents.
One study by Seaton et al10, suggested that PDL had no effect on P. acnes colonisation or sebum production (measured using the application of absorptive tape). They did however note upregulation of transforming growth factor beta (TGF-β). Given that this is a potent inhibitor of inflammation, this finding suggests that this laser may act through anti-inflammatory effects. It has also shown to inhibit CD4+ T-lymphocyte mediated inflammation. TGF-β may also induce keratinocyte growth arrest which could possibly interfere with comedone formation. Sami et al11 compared PDL/intense pulsed light (IPL) and LEDs in the treatment of 45 patients with moderate to severe acne. They found that a clearance of 90% of inflammatory lesions was achieved quicker with the use of PDL over IPL, which was more effective than LED.
The exact mechanism of how PDL works appears to be multifactorial. The photothermal effect on the sebaceous glands are achieved partly by heating of the dermal microvasculature secondary to the oxyhaemoglobin absorption. It is hypothesised that the generated heat leads to the induction of heat shock proteins, such as HSP70, which in turn could play a role in TGF-β production.
In summary, PDL is likely to work owing to both photochemical and photothermal effects and although the ideal exact parameters are not yet established and the studies have shown conflicting and inconsistent results. The debate on the true efficacy and role of PDL in acne continues with mixed opinions on its place and efficacy in acne.
Potassium titanyl phosphate
The 532 nm laser emits green light pulsed laser therapy, which penetrates deeper than blue light. It activates porphyrins, which target P. acnes as well as causing non-specific thermal injury to the sebaceous gland. It therefore exhibits a photochemical as well as mild photothermal effect. It has been shown to have short-term results on acne lesions with few side-effects. Four open-label studies have assessed the effectiveness of the potassium titanyl phosphate (KTP) laser in the treatment of acne. In a split-face, prospective controlled trial of 26 patients with moderate acne, Baugh et al12 reported that the KTP laser was a safe and effective method in treating acne lesions. Results lasted up to 4 weeks after treatment, with a 21 % reduction on lesion count at 4 weeks versus a 35% reduction at 1 week. Bowes et al13 carried out a prospective, split-face study of 11 patients and noted a 36% reduction of mild to moderate acne lesions in comparison to 2% in the control side. Yilmaz et al14 also supported the use of this laser in the treatment of mild to moderate acne in 38 patients. Their findings showed that there was no difference between once or twice weekly applications.Despite these studies, the results are generally short-term and this laser is not often used in the management of acne.
Infrared lasers
Infrared lasers penetrate deep into the dermis targeting water as their main chromophore. Water is the dominant chromosphere in the sebaceous gland, thus infrared lasers are thought to arrest the production of sebum and eliminate acne. Both the 1450 nm and 1540 nm lasers have been used in this manner15. Seventeen studies reported the use of these lasers, 12 were open-label and five were randomised.
1540 nm laser
The 1540 nm erbium glass laser is a mid-infrared laser and has effectively been used to treat acne lesions in four studies. A 78% reduction in acne lesions was observed in 25 patients after four treatments at 4 week intervals16. Kassir et al17 noted a similar reduction (82%) at 3 months in 20 patients who received treatments twice a week for 4 weeks. Angel et al18 demonstrated the longest clearance effects of the 1540 nm laser in a 2 year follow up. The mean percentage reduction of 18 patients treated with four treatments at 4-week intervals was 71%, 79% and 73% at 6, 9 and 24 month follow-up respectively. Inflammatory acne was shown to improve by 68% in 15 patients with moderate to severe acne treated four times at 2-week intervals; however, there was no reported change in sebum production19. Virtually no side-effects were reported with the use of this laser. It is likely this laser exhibits its effects through non-selective heating of the sebaceous glands.
The 1450 nm laser
This laser was first used in a study of 19 patients with inflammatory acne in which traditional therapies had failed. A fluence of 14 J/cm2 was used in three treatments at 4 to 6 week intervals and a 37% and 83% reduction in lesion count was observed after the first and third treatment respectively. Side-effects included transient erythema and oedema20. A randomised split-face trial was carried out to compare two treatment fluences by Jih et al. Twenty patients received three treatments at 3 to 4 week intervals. After one treatment, the percentage reduction in mean acne lesion count was 43% (14 J/cm2) and 34% (16 J/cm2), patients were followed up for 12 months and the reduction in lesion count was 76% (14 J/cm2) and 70% (16 J/cm2)21. Acne scarring and sebum production also improved.
The 1450 nm diode laser heats the upper mid-dermis to a depth of 500 µm and can result in thermal coagulation of the sebaceous lobule and the follicular infundibulum4. It is thought to improve acne lesions via heating the sebaceous gland and reducing its activity. Perez-Maldonado et al22 displayed an 18% reduction in sebum production (measured by sebutape scores) in eight patients treated with the 1450 nm diode laser for three treatments over a period of 6 weeks. Contrasting results were seen in 14 healthy subjects (without active acne), with this laser showing no significant reduction on sebum production23.
A split-face bilateral paired study treated 11 patients with the 1450 nm diode laser at a fluence of 11 J/cm2. One half was treated with a single pass consisting of stacked double pulses and was compared to a double pass treatment of single pulses. The stacking of pulses was more effective in reduction of acne lesion count compared to the multi-pass technique24. Lower fluences elicit less pain while still effectively treating inflammatory lesions. Single pulse multiple pass methods may have a reduced chance of cryogen-induced transient hyperpigmentation in comparison to the standard high fluence techniques.
Yeung et al25 supported that multiple pass/lower fluence can still retain efficacy but reduce post-inflammatory hyperpigmentation. Bernstein et al performed a randomised split-face trial of six patients with papular acne, comparing single pass high energy treatment (13–14 J/cm2) and double pass low energy treatments (8–11 J/cm2) for four treatments at monthly intervals. Single pass high energy had greater reduction in lesion count reduction (78% vs 67%), however the pain score was greater in the single pass group (5.6 vs 1.3)26.
The 1450 nm diode laser in combination with the 585 nm laser has been shown to be effective in the treatment of inflammatory acne, acne scarring and post inflammatory erythema in 15 patients. The addition of microdermabrasion to the 1450 nm diode laser showed no significant benefit for treatment effectiveness or pain in a randomised split-face trial of 20 patients27.
Despite the results of the aforementioned studies, this laser is associated with a relatively high degree of pain and discomfort and is no longer considered a laser of choice in the treatment of acne by many laser dermatologists worldwide.
Photodynamic therapy
Photodynamic therapy (PDT) involves the use of a photosensitiser, which is taken up by the pilosebaceous unit and undergoes metabolism through the haem-synthesis pathway resulting in the production of protoporphyrin IX28. The activation of this pathway leads to the production of free radicals and singlet oxygen which are cytotoxic and accumulation of this in the epithelium and pilosebaceous unit lead to elimination of the P. acnes and modulation of the sebaceous gland and infundibulum. P. acnes cultures grown in the presence of ALA led to a 5-fold decrease in culture viability after three illuminations of high intensity blue light. For PDT to be effective light, oxygen, and a photosensitiser are required. 5-aminolevulinic acid or methylaminolevilunate (MAL), indocyanine green (ICG), and indole-3-acetic acid are used as photosensitisers. A light source can be a light emitting diode, fluorescent lamps, lasers, sunlight, xenon flash lamps, arc lamps, and filtered incandescent lamps. P. acnes photo-inactivation can be altered depending on the concentration of porphyrins which is governed by the type of acne lesion, effective fluence, wavelength of the photons emitted and the temperature29.
Twenty studies using PDT in acne were published, (11 randomised trials and nine open-label). An IPL source was used in four studies (randomised split-face, open-label, randomised open-label, and a split-face pilot study). Aminoluevelunic acid (ALA) was used in four cases and MAL in one case. Yeung et al30 noted a 65% reduction in inflammatory lesions after 12 weeks following PDT in comparison to 23% reduction when using IPL alone. Similar findings were found by Rojanmatin et al31 at 12-week follow-up in a split-face trial. The PDT side had an 87% reduction in lesions in comparison to 66% reduction with IPL alone. Another split-face trial using ALA with IPL was studied by Santos et al32 in 13 patients with 10 out of 13 patients using the combination treatment showing marked improvement in comparison to the IPL alone group. Different modalities were compared by Taub et al33, they compared IPL, IPL and bipolar radiofrequency (RF), and IPL and blue light for activating ALA-induced protoporphyrin IX. ALA-PDT activation with IPL provided the greatest and longest lasting effects in comparison to RF-IPL and blue light.
Four studies used long-pulse PDL, (one randomised controlled split-face single blinded trial, one cross-sectional comparative controlled prospective study, one split-face open-label study, and one prospective randomised study). MAL was used in conjunction with long-pulse PDL in two studies and a significant reduction in lesion count in the PDT-treated areas was seen by Haersdale et al34. A reduction in both inflammatory and non-inflammatory lesions was noted; however erythema and oedema were reported as significant side-effects.
An interesting study by Hongcharu et al35 with ALA followed by irradiation with red light showed histological evidence of sebaceous gland hypotrophy with glandular destruction. Furthermore, ALA-PDT decreased P. acnes fluorescence, a marker for bacterial colonisation, as well as sebum secretion post therapy. Despite such encouraging findings, some studies using ALA followed by red light have failed to show any significant reduction in sebum production or P. acnes colonisation35.
Red light was used in seven studies. Two randomised controlled trails, investigator-blinded, controlled trial, and a randomised controlled trial. Two studies used ALA plus red light, which saw a significant reduction in lesions.
Of 18 patients studied by Taub et al33, 11 were noted to have a 50% improvement and five to have a 75% improvement. Side-effects included erythema and peeling. Goldman et al36 followed 22 patients up for two weeks and noted an improvement in lesion count with no reported side-effects. There was a greater response in the ALA-blue light group compared to the blue light group alone. The same author used short contact ALA for 1 hour with either an IPL source or blue light with relative clearance of the inflammatory lesions. Gold et al also used short contact ALA of 30–60 minutes in combination with blue light in moderate-to-severe inflammatory acne and noted a response rate of 60%.
Blue light was also used in combination with ALA in two studies. Itoh et al37 used halogen light with a filtered band of 600–700 nm in combination with ALA in 13 patient with all patients showing an improvement in their inflammatory component.
MAL is a lipophilic derivative of ALA and may therefore have better penetration. Its use as a photosensitiser in acne therapy was used in two European studies. The first by Wiegell and Wulf38 and the second study by Horfelt et al39. Both studies showed a modest improvement in acne lesions with occlusion time of 3 hours.
Intense pulsed light
[pull_quote align=”right” ]IPL technology works in single- and burst-pulse modes. In the single-pulse mode, the fluence will be delivered in single shot, whereas in burst-pulse mode fluence is divided into a series of pulses with a delay between the pulses.[/pull_quote]
An IPL device delivers an intense source of light, the wavelength of which can be modified via the use of filters. The generated pulsed light is polychromatic and non-coherent and the emitted light can be tailored to the treatment by alteration of the filtered light, pulse duration, and fluence. IPL technology works in single- and burst-pulse modes. In the single-pulse mode, the fluence will be delivered in single shot, whereas in burst-pulse mode fluence is divided into a series of pulses with a delay between the pulses. The theory of treating acne lesions with IPL is based on the photochemical and photothermal (higher settings) effects on the bacterial-derived porphyrins, as well as the inflammatory cells that mediate an inflammatory cascade, heating of the sebaceous glands, and small vessels associated with the process40. The photochemical effects are likely to occur owing to the blue and red range of light emitted by the IPL; whereas the infrared range of light has more of a photothermal effect on the sebaceous glands and dermal vasculature. IPL was used in nine studies with mixed results. Elman et al used 430–1100 nm source in patients with moderate acne and saw a 74% and 79% reduction in inflammatory and non-inflammatory lesions respectively, following twice weekly therapy for 4 weeks15. Lee et al carried out a split-face control trial in patients with mild to moderate acne and noted a significant reduction in both inflammatory and non-inflammatory lesions in comparison to no treatment41. A further split-face trial with the use of Benzoyl peroxide with or without IPL did not show a significant difference in comparison to using IPL alone. Dierickx et al demonstrated a clearance rate of 72% at 6 months post therapy42. IPL was combined with RF and results showed that the mean lesion count was reduced by 47%; it was suggested that this reduction was owing to reduction in sebaceous gland size and decreased peri-follicular inflammation. Their findings were based on post treatment skin biopsies43. In comparison with other modalities, IPL has been found to be less effective than PDL but more effective than blue or red light.
Photopneumatic therapy
Photopneumatic therapy (PPX) combines pneumatic energy and broadband light (400–1200 nm) encompassing the blue wavelength 410 nm, which is the wavelength that is greatest for porphryin absorption. The suction acts to lift the contents of the dermis bringing them closer to the skin surface, thus making energy transfer more effective. The epidermis and therefore melanin in the epidermis is spread out and the photopneumatic treatment reduces adverse effects on the epidermis, such as pigmentary changes44. In addition, the suction applied owing to negative pressure may help to rid comedones of their contents. Therefore, the action of PPX involves a combination of thermal and vacuum-related mechanical effects. A number of studies have used this technology in the treatment of acne. In one study by Shamban et al44, 56 patients with mild to severe acne were treated with PPX, and found to have a 50% clearance of lesions after one session and 90% after four sessions. Omi et al45 observed ultrastructural changes to the pilo-sebaceous unit after PPX treatments. Histologically, the authors were able to observe extrusion of comedone contents from the infundibulum and thermal injury to the bacteria and pilosebaceous apparatus, supporting the theory that PPX decreased sebaceous gland activity. No adverse effects were reported.
[pull_quote align=”left” ]The treatment of acne vulgaris often requires combination therapy and a tailored treatment regimen to each case.[/pull_quote]
Gold and Biron46 demonstrated efficacy with PPX in seven patients treated with a total of four treatments at 3 week intervals. A larger study by Wanitphakdeedecha et al47 involving 20 patients who were treated at 2 week intervals demonstrated modest improvement in acne lesion counts.
In a prospective, multicentre, clinical trial involving 41 patients with mild-to-moderate acne, Narurkar et al48 reported a 69% reduction in the inflammatory component, in contrast to 41% reduction in the non-inflammatory component of the disease. There were no adverse effects caused by the treatment with mild discomfort and transient erythema being the most reported side-effects. In the author’s experience, this treatment is effective in the mild to moderate cases of acne and in combination with topical therapy.
Discussion
The treatment of acne vulgaris often requires combination therapy and a tailored treatment regimen to each case. Despite advances in our understanding of the disease and the wide array of topical and systemic therapies available, in many cases the disease can still be resistant to medical therapy and hence light-based treatments may offer an alternative or act as adjuncts.
Light-based technologies can largely be based on their photothermal effect, predominantly on the sebaceous glands and their associated dermal vessels, or on their photochemical effects by targeting the coproporphyrins produced by P. acnes leading to cell death. The photochemical effects can be produced with or without the application of a photosensitiser such as ALA, although most of the current evidence points toward the PDT-mediated effects of therapy on acne. This is particularly the case when sustainable duration of the results are taken into consideration. Unfortunately, the side-effects with PDT appear to be the main limiting factor for their use in the treatment of acne in the majority of the cases.
Blue and red light therapy in the form of LEDs has shown efficacy, with the former exhibiting a photochemical effect and the latter a predominantly immunomodulator and anti-inflammatory effect in addition to some photothermal effects. These effects appear to be much more superior again when combined with a photosensitiser (i.e PDT effect as opposed to LED alone).
IPL has shown to be effective with its broadband range, having a combination of photochemical and photothermal effects, although the studies have shown that IPL combined with a photosensitiser is superior to IPL therapy alone. Furthermore, when compared against PDL, the latter has shown a superior effect.
Studies using the PDL in acne have shown conflicting results too, although evidence of TGF-β upregulation has been demonstrated, this does not appear to be sufficient in controlling the disease in many cases. Both PDL and IPL have a place in acne treatment today, particularly in the cases where it is associated with acne-induced facial erythema. This is similarly the case with the KTP laser.
Infrared lasers are less widely used nowadays in acne owing to the associated pain and associated discomfort.
PPX is a relatively new technology in the treatment of acne and appears to be effective in mild-to-moderate cases combining both photochemical effects with mechanical extrusion of comedonal contents in addition to a mild photothermal effect.
Despite the large number of studies published using light-based technologies in acne, the results show mixed results and firm conclusions are difficult to draw. Many studies were open-labelled or lacked optimal methodological qualities and involved a relatively small number of patients. A lack of objective assessments of outcome further contributes to the somewhat tempered enthusiasm for the use of this technology in acne. Larger, randomised, controlled trials with clear objective outcome measures and consistent agreed settings, which vary hugely among the published studies, would be needed.
Conclusion
Laser and light based therapies may act as alternative treatments for patients that have not responded or are not suitable for medical therapy. The effects of light-based therapies rely on photochemical, photothermal, or the combination of both effects. For light-based therapies to be effective, ideally targeting both the P. acnes as well as the sebaceous glands appears to be the best approach. To date, most of the studies were underpowered or showed inconsistent results with a relatively small number of patients involved. Optimal parameters are yet to be established. In the author’s opinion, light-based therapies often offer very effective treatment when combined with medical therapies in selected patients.