Daniel Sister discusses how growth factors can be used in a range of medical procedures to improve our health and longevity, including lipofilling, knee surgery, and vascular treatments.
What is Ageing? How can we define it? Is it just getting older? Is it the number of years since birth or is it the way you look, feel, and live?
Since the beginning of recorded history, mankind has searched for a way to slow down and possibly even reverse the process we know as ageing.
More than one in three adults under the age of 50 now shops for anti-ageing products including better medicine, proper nutrition, vitamin and mineral supplements, anti-ageing hormones, and aesthetic/cosmetic treatments. As more than 80 million ‘Baby Boomers’ grow into their 50’s, 60’s, and 70’s, they all share a common dream: to stay active, to be able to compete with younger generations in the work place, and look good.
Life expectancy has increased dramatically over the last several decades. Once women reach the age of 65, they can expect to live to the age of 80 years and even to 87, and if men make it to 75 they can expect to reach 85 years of age.
According to experts from the United Nations (UN), seniors will outnumber children for the first time in history by 2050. The UN predicts that there will be nearly 2-billion citizens aged 60 and over by the mid-century, and that the growth of the elderly population will have profound effects on the economy.
However, with living longer we face different issues. Our bodies aren’t what they used to be and our hormone production begins to decline as we approach middle age. On the surface, lines, wrinkles, and folds are more pronounced and hair may thin and fall out; joints, tendons, and ligaments are also weaker.
So what is a baby boomer? Stated very simply, sociologists and the media define baby boomers as those born between (and including) 1946 and 1964. The ‘grey’ population is the fastest growing market in the EU, UK, and US.
Currently over 42% of the skincare, make up, personal and oral hygiene market is made up of people over the age of 45 years throughout both the EU and US populations.
Technology and medical knowledge are doubling every 3 and half years. By 2020 there will be 64 times more knowledge to fight the ageing process. We have more in-depth knowledge of how our hormones work and how to balance them. Botulinum toxin was not on the market 20 years ago, neither were dermal fillers, but now lasers, ultrasound, radiofrequency, and LED have become common treatments.
The motivation behind all this activity is clear: no one wants to grow old in a culture that equates youth with desirability. Men and Women alike strive to be socially attractive and economically marketable for as long as possible.
The discovery of growth factors
In the author’s opinion, the most important advance in the fight against ageing is the discovery of growth factors.
In 1986 the Nobel Assembly at the Karolinska Institute awarded the Nobel Prize in Physiology or Medicine jointly to Stanley Cohen and Rita Levi-Montalcini for their discoveries in 1953 of two growth factors. The neural growth factor (NGF) and epidermal growth factor (EGF) were the first of many growth-regulating signal substances to be discovered and characterised.
During the course of his studies of NGF, Stanley Cohen observed an unexpected acceleration of development when he injected salivary gland extract into new-born mice. The explanation was that the salivary gland extract contained another growth factor apart from NGF. Cohen termed this substance epidermal growth factor (EGF) because it could stimulate the proliferation of epithelial cells in skin and cornea.
Today, we know that cells communicate with each other via signal substances (cytokines and hormones). Initially it was believed that hormones were only produced in specialised endocrine glands, from which hormones, such as growth hormone, were released into the blood stream. Biochemists disagree as to which molecules should be termed cytokines and which hormones. As we learn more about each, anatomic and structural distinctions between the two are fading.
During the last decade, several growth factors have been isolated and characterised by different research groups. It has now become clear that many cell types synthesize signal substances or hormones that have their effects both on their cell of origin, as well as on neighbouring cells.
Platelet rich plasma
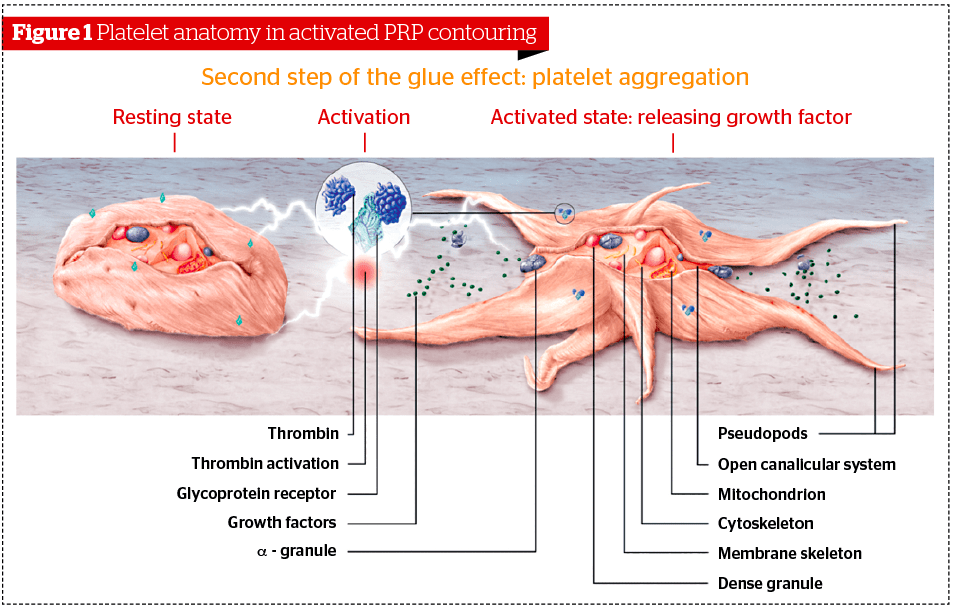
Platelet rich plasma describes a fraction of the plasma with a high concentration of platelets. Platelets are formed when cytoplasmic fragments of megakaryocytes (which are large progenitor cells in the bone marrow and the source of platelets), are released into the circulation as they age. They are round or oval in shape, approximately 2 µm in diameter. Platelets lack nuclei but contain organelles and structures such as mitochondria, microtubules, and granules.
Platelets contain two unique types of granules—the alpha-granules and dense granules. Alpha-granules contain a variety of haemostatic proteins (coagulation proteins), as well as growth factors and cytokines. Dense granules contain factors that promote platelet aggregation (ADP, calcium, serotonin). Cell activation of platelets causes the discharge of granule content. In other words, platelets require activation in order to begin the cascade of events that lead to collagen restoration and growth. This activation must occur at the tissue level (where the platelets aggregate and adhere to collagen at the site of grafting1.
The platelet is metabolically more active than the red blood cell and has a variety of functions. It is well known that platelets play an important role in the formation of the blood clot. But platelets also store and transport several chemicals, growth factors, cytokines, chemokines (pro-inflammatory activation-inducible cytokines), serotonin, epinephrine, histamine, and other proteins such as adhesion proteins2.
Most reviews on this topic focus on only the growth factors contained within the alpha granules of the platelet that are released upon platelet activation3. It is important to understand, however, that if the platelets aren’t suspended with biologic levels of other constituents of plasma such as leukocytes, other cytokines, and fibrin (the matrix), the graft is either less or not effective4. If fibrin levels are too high, or platelet activation occurs prior to collagen binding, the graft is also inhibited. Other functions of platelet activation and the subsequent cascade of events that occur include cytokine signalling, chemokine release, and mitogenesis5.
In the wound healing environment, platelets will degranulate within 10 minutes of the formation of the clot, releasing growth factors into the local environment; 95% of the pre-synthesized and existing platelet growth factors are present in the wound within the first hour. However, normal platelets will continue to synthesize and release growth factors over the next 7–10 days, thus supporting angiogenesis, collagen production, and other aspects of wound healing.
Alpha granules
Of primary interest to the clinician are the three adhesion molecules and seven growth factors present in the alpha granule3, including:
- Three isomers of platelet-derived growth factor (PDGF)
» Chemoattractive to mesenchymal stem cells and endothelial cells
» Differentiation for fibroblasts and osteoblasts
» Up-regulate effects of other growth factors on cells such as macrophages
» Mitogenes of mesenchymal stem cells and promote the synthesis of the extra cellular matrix - Transforming growth factor (TGF)-[1 and 2]
» Promotes cell mitosis
» Favours the synthesis of collagen and significantly increases type I collagen production in tendon
» Protect fibroblast
» Stimulation of DNA synthesis and proliferation of various types of cells - Vascular endothelial growth factor (VEGF)
» Stimulates angiogenesis and chemo attractive for osteoblasts
» Epidermal growth factor (EGF)
» Important role in the regulation of cell growth, proliferation, and differentiation by binding to its receptor EGFR
» Induce epithelial development and promote angiogenesis
» Stimulates proliferation and differentiation of epidermis cells - Platelet factor 4 (PF4)
- Interleukin (IL)-1
- Platelet-derived angiogenesis factor (PDAF)
- Platelet-derived endothelial growth factor (PDEGF)
- Epithelial cell growth factor (ECGF)
- Insulin-like growth factor (IGF)
- Osteocalcin, osteonectin, fibrinogen, vitronectin, fibronectin, and thrombospondin (TSP)
In addition, the activated thrombocytes have a multitude of signalisation molecules: CD9, CD-W17, CD41, CD42a-d, CD51, CD-W60, CD61, CD62P, CD63.
Is PRP efficient?
Since the discovery of growth factors, a multitude of medical studies have been published (over 11,500 on Pubmed covering all different medical fields).
During the inflammatory phase, the functions of activated platelets include:
- Anti-microbial
- Adhesion
- Aggregation
- Pro-coagulation and clot retraction
- Cytokine signaling
- Chemokine and growth factor release.
There is now evidence to suggest that at certain concentrations, or dose response curves, platelet rich plasma grafts may be anti-inflammatory or pro-inflammatory in certain tissues6.
Following the initial inflammatory phase, which typically lasts for 2 to 3 days, fibroblasts enter the site and begin the proliferative phase. Low pH and low oxygen levels stimulate fibroblast proliferation in the injury site. Fibroblasts become the most abundant cell by day 7. They are responsible for deposition of collagen and ground substance.
The proliferative phase and fibroblast function:
- Aid in wound contraction
- Peak from day 5–15
- Can last for weeks
- Fibroblasts then differentiate into myofibroblasts
- Actin contracts making wound smaller.
Low pH and hypoxemia also stimulates neovascularization as proven by Li and Yawei in their study, ‘Fibroblast proliferation due to exposure to a platelet concentrate in vitro is pH dependent’7. Neo-vessels begin to form at approximately day 5 to 7 and this process proceeds until the neo-vessels disappear near completion of the remodelling phase.
The remodelling phase
During this phase (which can last over a year), collagen matures and strengthens. Tissue repair starts when the production and break down of collagen equalizes. During this period, type III collagen is replaced by type I collagen, reorganization occurs, and the blood neo-vessels disappear5.
Tissue biotensegrity—refers to a dynamic construction of compressive and tensional forces acting on, and through, multiple levels of organization to maintain or repair tissue homeostasis8–10.
PRP use in anti-ageing medicine
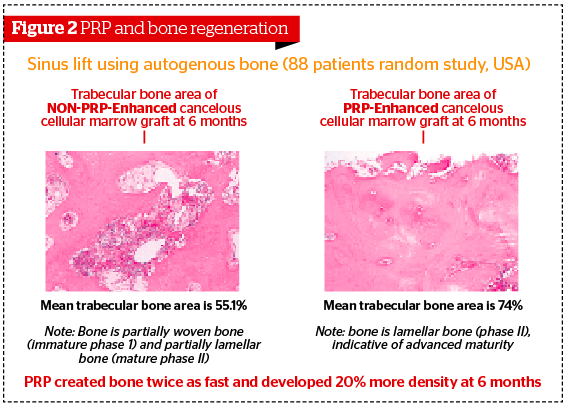
It is a well-documented and efficient procedure for implantology11,12, since Marx showed in 1970 a 20% increase of density in the trabecular bone. As well as a reduction of 40% to healing time and 80% of pain with PRP.
Hesham El-Sharkawy et al. evaluated this effect in periodontal tissue6. The conclusions were that PRP is a rich source of growth factors and promoted significant changes in pro‑inflammatory cytokine/chemokine release. LXA4 was increased in PRP, suggesting that PRP may suppress cytokine release, limit inflammation, and thereby promote tissue regeneration.
One study demonstrates that one local infiltration of PRP associated with a submaximal eccentric protocol can improve symptoms of chronic jumper’s knee in patients non-responsive to classical conservative treatments13.
A retrospective evaluation of patients receiving a single PRP injection for chronic mid-substance Achilles tendinopathy revealed that 78% had experienced clinical improvement and had avoided surgical intervention at 6-month follow-up14.
Application of a single dose autologous PRP adjunct to surgical repair improved results in tendon-to-bone healing, assessed by histological and biomechanical testing in a rat model of acute RCT, when tested at 3 weeks compared to controls15. Another randomised control trial of athletes suffering from high ankle sprains proved the benefit from ultrasound-guided PRP injections with a shorter recuperation time (RTP), re-stabilization of the syndesmosis joint, and less long-term residual pain.
Olena Virchenko and Per Aspenberg noted, in a rat achilles tendon transection model, that one postoperative injection resulted in increased strength after 4 weeks. This effect was not seen with the use of botox at the site16.
Mishra performed an in vitro study which determined the effect of a platelet concentrate medium on the proliferation of human skin fibroblasts—the cells responsible for deposition of collagen. Buffered PRP was shown to augment human fibroblast proliferation when compared to control17.
As well as in cartilage dysfunction, intra-articular PRP injections into the knee for symptomatic early stages of osteoarthritis show a significant reduction in pain and improvement in function after 12 months, which can be further improved at 18 months by annual repetition of the treatment18.
The application of autologous platelet rich plasma gel in cartilage regeneration show that PRP may provide a suitable environment for the proliferation and maturation of chondrocytes, and can be used as a promising bioactive scaffold for cartilage regeneration.
El-Sharkawy et al., measured platelet derived growth factor (PDGF)-AB, PDGF-BB, transforming growth factor-b1, insulin-like growth factor-I (IGF-I), fibroblast growth factor-basic (FGF-b), epidermal growth factor (EGF), vascular endothelial growth factor, interleukin-12 (p40/70) and, regulated on activation, normal T‑cell expressed and secreted (RANTES) levels by enzyme-linked immunosorbent assay.
In the study, PRP led to significantly increased levels of growth factors and significantly suppressed inflammation. IGF-I levels in PRP in this study were not significantly different from the cyclolignan picropodophyllin (PPP), suggesting that other cell types could be responsible for the release of this growth factor6.
Scarpone reported on a prospective study carried out on 14 patients with shoulder pain. The patients all had rotator cuff tears with no significant AC joint thickness with impingement and no other significant symptomatic pathology such as labral tears, gleno-humeral arthrosis, or gross instability. All of the patients failed non-operative treatments such as NSAIDs, physical therapy, and corticosteroid injections and all were considering surgical options. Of the 14 patients, 12 had statistically significant improvements in their pain scale, their strength, and endurance at 8 weeks. Of the 12 patients, six had radiographic evidence of healing of their tendinopathy on MRI at 8 weeks. Of the four patients who were considering surgery because of persistent pain, only two went on to have rotator cuff surgery. No significant complications were noted19.
Aesthetic surgical procedures
The first exciting studies in this field came from Eppley and Brown but now more complete studies validate the concept20–22.
A retrospective analysis was used with regard to recovery time and the aesthetic improvement after treatment among four groups of patients: those treated with fat grafting only (Group I), those treated with fat grafting and PRP (Group II), those treated with a minimal access cranial suspension (MACS)-lift and fat grafting (Group III), and those treated with a MACS-lift, fat grafting, and PRP (Group IV).
The conclusion was that the addition of PRP to a lipo-filling procedure resulted in a significant drop in the number of days needed to recover before returning to work or to restart social activities23.
Tissue culture studies performed by du Toit et al. for use in dermal regeneration confirmed the potent mitogenic stimulation of human fibroblasts, keratinocytes, chondrocytes, neural tissue, and myoblasts24. In recent studies, injection of PRP in the face and neck for revitalisation obtained good results25.
With the use of PRP, a prospective, single-blind pilot study comprising 80 full-thickness skin punch wounds (4 mm diameter) was conducted on the thighs of eight healthy volunteers. With each subject serving as his or her own control (five punch sites per leg), PRP was applied topically on one thigh, while an antibiotic ointment and/or a semi-occlusive dressing was applied on the other thigh. On day 17, the percentage of closure was 81.1% for the PRP-treated sites and 57.2% for the control sites. Also, the PRP wound closure velocities were significantly faster than those of the controls (P=0.001). When the platelet count in the gel was more than six times the baseline intravascular platelet count in some subjects, epithelialization and granulation formation appeared 3 days earlier in the PRP-treated group26.
The ageing process on the face is a complex interaction between a variety of facial elements. The process can be described as a cascade effect, which happens in four main facial layers:
- The bone: bone resorption on the orbits and jawline
- Muscle: tightening with age
- Fat pads: melting and sliding
- Skin: collagen and ECM.
A study conducted by Amgar27 used biometric parameters for scientifically measurable means of assessing the results from the PRP injections. The study also demonstrated that the effects of one PRP treatment could last for up to 10 months.
Use in vascular treatments
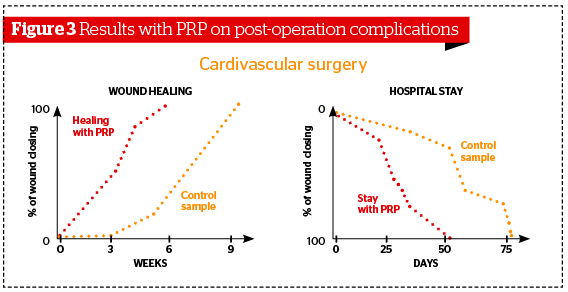
Platelet rich plasma was first used in cardiac surgery by Ferrari et al., in 1987 as an autologous transfusion component after an open heart operation to avoid homologous blood product transfusion28.
The results of surgical treatment of 36 patients suffering inoperable types of the peripheral arteries occlusion were analysed. In 18 patients, the algorithm of intraoperative ultrasound duplex scanning was applied and surgical interventions were performed using optimised procedures. As a second stage, the PRP-therapy was conducted, since the second post-operative day all the patients have performed the elaborated complex of physical exercises directed on shin and hip muscle strengthening. Optimisation of the lower extremities indirect revascularization methods have permitted to increase the rate of treatment positive results from 55.6% to 88.9% and to reduce the unsatisfactory results (from classical treatment) rate from 44.4% to 11.1%.
PRP-concentrate constitutes a potent cell biological activator of the VEGF, and improves metabolism and microcirculation in muscles and cells of the skin29.
The safety issue
Regarding the question of carcinogenesis, growth factors only act on cell surface receptors, do not enter the cell, and do not cause DNA mutation. There is no plausible mechanism by which growth factors would result in neoplastic development, and there have been no reports of this in the literature.
The concentration of growth factors is 50% above whole blood and not in concentrations that should cause concerns. Additionally they are in natural ratios to each other, such that the signalling factors are not above normal levels. Man-made biologics are many times more concentrated than that.
Knowledge has improved a lot since the discovery of growth factors and the beginning of PRP treatments and we know much more now on how to obtain an efficient volume of PRP:
- Complete and easy handling single-use kits for collection
» Minimising the number of manipulations
» Ensuring a full aseptic technique with a closed system (risk of contamination when obtaining by traditional pipetting)
» No vacuum tubes as the pressure to withdraw blood are harmful to platelets membranes - Sufficient volume: it was found that platelet concentration of growth factors will be dependant:
» Upon the amount of whole blood used
» Platelet recovery efficiency
» The final volume of plasma in which platelets are suspended.
Most kits on the market use tubes of 8 to 10 cc, which give a volume of ‘PRP’ close to 2–4 cc. Others are taking up to 50 cc of patient’s blood making the procedure uncomfortable for the patient and dramatically increasing the costs.
The harvesting tube dimensions are very important, in particular the diameter as the practitioner must avoid self-activation at all cost. This would occur due to the increase in concentration and platelet aggregation that follows due to their physical proximity. Within the tube, the acceleration process is uni-directional and varies with the length of the tube by increasing linearly with the distance to the rotation axis. Therefore, it makes sense to use harvesting tubes of 20 cc. The following is a list of what the author looks for when preparing an efficient batch of PRP:
- Avoiding haemolysis (especially aesthetics, red spots, and inflammation)
- Reducing additions/avoid separating gel (degradable variable effectiveness, possible contamination). Avoid adding non-autologous products
- Controlling the activation: use of a nontoxic activator (CaCl2) to benefit from the effect of concentration of growing factors and no pipetting
- Acceleration G-force and time of centrifugation30–32
» Strong acceleration has to be avoided because platelet membranes can be impaired. It has been established that excessive acceleration decreases the integrity of the platelet membrane some of which are then activated. Thus, for more than 400 G values, 5% of platelets are activated and 40–70% of them become activated at 3000 G - Sufficient and optimal concentration6,33
» There is emerging evidence to suggest that PRP grafts in the 4–6 fold range have more anti-inflammatory mediators and effects and are clinically relevant and useful for most situations. PRP grafts in the 8–13 range may be pro-inflammatory in nature and that higher concentrations might have a paradoxically inhibitory effect. Weibrich et al32., observed an advantageous effect with platelet concentrations of approximately 106/µL. Further, they state that higher concentrations might have a paradoxically inhibitory effect - Precise harvesting and reproducible segregation
» Unfortunately, if we can find very strong and positive studies, there are also some negative ones. In most cases those studies analysed a relatively small number of cases. In general, the results vary depending on the practitioner, the protocol, as well as the harvesting technique and kit used, even more so in cosmetic/aesthetic medicine. Those conditions explain why all PRP and plasma treatments are not created equal and why the medical community is divided.
In all other medical disciplines, the plasma is either injected deep or placed in situ (implantology, surgery, sport medicine). However, in aesthetic medicine it was (and often still is) mainly injected superficially (mesotherapy). This could be another explanation for the various results, along with different preparation methods.
Based on the previous considerations, the author recommends the following when harvesting and using PRP:
- Using a 20 ml harvesting kit with a physical separation between RBC and plasma (without any chemical separation)
- A low G force and a longer spinning time (8 minutes)
- Injecting at different depths: deep (contact to periosteum), medium deep then superficially
Using the total plasma as platelet poor plasma is also important as demonstrated by a Korean study34, where the effects of activated platelet-rich plasma (aPRP) and activated platelet-poor plasma (aPPP) have been investigated on the remodelling of the extracellular matrix, a process that requires activation of dermal fibroblasts. aPRP and aPPP both stimulated cell proliferation, with peak proliferation occurring in cells grown in 5% aPRP. Levels of PIP were highest in cells grown in the presence of 5% aPRP. Additionally, aPRP and aPPP increased the expression of type I collagen, MMP-1 protein, and mRNA in human dermal fibroblasts.
The author’s results to this date on a very large cohort of patients are definitely positive. All were treated with the same protocol (deep, medium deep, and superficial injections of the full plasma: about 10 ml of PRP and PPP). None were asked to return if not specifically pleased with their results.
Once cleaning the data of patients living abroad, who became pregnant, or had other good reason not to return:
- Total patients treated: 328
- Total number of treatments: 921
- Patients treated with only one session: 55
- Patients with two sessions: 89
- Patients with more than two sessions: 184.
Conclusion
In reading the medical literature in regards to plasma, we will find different names and definitions, such as platelet leukocyte gel, PRP, platelet rich plasma gel, and platelet concentrate depending on where it is used and what for. But why and how does plasma (and growth factors) work for so many different problems?
As stated by Mr. A. Ghanem (Blizard institute/Barts and London School of Medicine) all circulating growth factors from all endocrine system are to be found in the plasma; therefore, they are able to target and assist different issues.
As we age, not only are we losing collagen (quantity and quality), developing a poorer skin vascularisation, and experiencing muscles shrinking but we are also losing bone structure especially around the orbit and jaw line. We also start to suffer from arthrosis. Our tendons and ligaments are not as resistant as they were. Hair begins to thin and fall out. Nevertheless, we do now have a totally safe, versatile treatment (stand alone or combined with surgery, botulin toxin, dermal fillers, lasers, chemical peelings, or implants) that will address all these issues.
Based on the author’s results, using the whole plasma and injecting deep, perhaps the term PRP should be replaced by a more comprehensive definition of blood plasma therapy.