Background: Over the years, there has been no 100% effective treatment for acne vulgaris (AV) and post acne scars. However, recently, new modalities for non-compliant, non-responder patients and those suffering from acne scarring have been developed. These include energy based treatments, such as the 585 and 595 nm pulsed dye lasers, the 1450 nm diode laser, the potassium titanyl phosphate laser, intense pulsed light sources, radiofrequency devices, and photodynamic therapy using 5-aminolevulinic acid and indocyanine green for AV or ablative and non ablative laser skin resurfacing for post acne scars.
Methods: The aim of writing this article is to review information about pathogenesis of acne and acne scarring, as well as energy based potential modalities.
Conclusion: Energy-based treatment options for acne and acne scars can be an alternative to medical modalities for non responders; those who have severe acne and are concerned about oral medications owing to potential adverse effects, or be used in combination with a topical medication. The goal of any modality in acne scars is not perfection; rather it is making scars less visible.
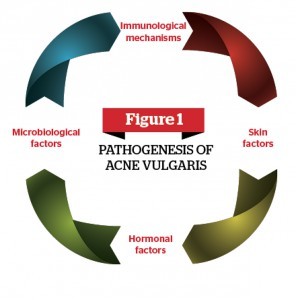
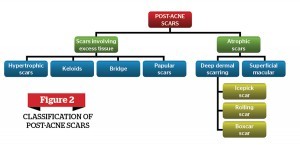
Acne vulgaris (AV) is a skin disorder of the pilosebaceous apparatus, which refers to hair follicles and their attached glands. Pathogenesis of AV is multifactorial, including hormonal, microbiological, and immunological mechanisms (Figure 1)1-2. Post-acne scarring is a process in which the collagen in the skin is damaged from inflammation; resulting in permanent texture changes and topographic depressions (Figure 2)3.
Though acne scarring is permanent, it can be treated. No treatment has been 100% effective, but the best result is improvement. Treatment of scarring may require many different modalities of treatments, depending on the kind of scarring present. It is important that all the acne is inactive before treating the scarring4.
Laser and light-based therapies for acne vulgaris
Lasers/light-based devices may offer an alternative and adjuvant to conventional acne treatments in non‑compliant, non-responder patients or in antibiotic resistance patients. Over the past decades, many types of light devices were introduced to treat and improve acne symptoms5.
Ultraviolet A/B
Improvement of acne was reported in 70% of patients after sunlight exposure6. Ultraviolet-A (UVA) and UVB therapy was found to have some beneficial effect, but it is potentially carcinogenic.7
Blue light and red light
Porphyrins are involved in processes of prokaryotic and eukaryotic cells, such as photosynthesis, biological oxidation, respiration, rearrangement of the carbon backbone, and sulphate reduction. P. acnes produce porphyrins, most notably on the nose and the forehead. The 407 to 420 nm band has the strongest porphyrin photo-excitation coefficient and blue light is the highest photo-activator of endogenous porphyrin component of P. acnes. However, blue light has poor skin penetration8. Red light, in contrast, has deeper penetration, up to the sebaceous glands, and also has anti-inflammatory properties9. Seventeen patients received eight sessions with the Silk’n Blue (Home Skinovations Inc., Richmond Hill, ON) device over a 4-week period. Follow-up visits were at 1 month and 3 months, respectively. A statistically significant decrease in mean acne counts from baseline was observed11. Many studies for the treatment of mild to moderate acne show the efficacy of blue light, or combination of both blue and red light12-13.
Potassium titanyl phosphate laser
In one study, 38 subjects were divided into two groups; one group was treated once weekly and the other twice weekly. One half of face was treated with 532 nm KTP and the other half was left untreated. They were evaluated at the beginning of the study, and then again 1 and 4 weeks after the last session with the Michaëlsson acne severity grading score (MASS). A significant improvement was seen in the second group who were treated twice weekly14.
The 532 nm KTP laser could penetrate and activate porphyrins to target P. acnes. It targets sebaceous glands with non-specific collateral thermal injury. It is well tolerated, safe and effective, with positive results up to 4 weeks post-treatment14-15.
Pulse dye laser
The efficacy of pulse dye lasers (PDLs) was demonstrated in a randomised, controlled, single-blind, split-face clinical trial of 40 patients with facial acne. They received one or two non-purpuric PDL sessions to half of the face (fluence of 3 J/cm2). Serial blinded clinical assessments from baseline to 12 weeks between treated and untreated sides of the face showed no significant difference16.
PDL 585 nm laser targets oxyhaemoglobin selectively and induces photo-thermolysis of the inflammatory dilated vessels. Porphyrins are activated to produce phototoxic effects by the delivery of coherent yellow light16. In another study, 80 patients were randomly divided in a 1:2 ratio and received only clindamycin 1%-benzoyl peroxide 5% hydrating gel C/BPO alone or in combination with PDL treatment (wavelength 585 nm, pulse duration 0.35 ms, energy fluence 3 J/cm2, spot size 7 mm), and were evaluated at baseline and at 2 and 4 weeks after initial treatment. Findings did not support the benefit of PDL treatment in acne vulgaris17. Also, Seaton et al18 suggest that PDL does not have an effect on P. acnes colonisation or sebum production. However, they revealed that the potent stimulator of neocollagenesis and a potent inhibitor of inflammation is the upregulation of transforming growth factor-β (TGF-β). So, its efficacy depends on its local anti-inflammatory effects. A randomised pilot study comparing a non-ablative, fractional 1550 nm laser versus a 595 nm PDL for facial erythema in 12 patients showed significant improvement results in both modalities for the treatment of acne erythema19.
Infrared lasers
Low-level laser (light) therapy (LLLT) is a fast-growing technology in treating acne. During LLLT, adenosine triphosphate, nitric oxide release, electron transport, reactive oxygen species increase, blood flow, diverse signaling pathways, and stem cells are activated, allowing increased tissue repair and healing20. Water is the dominant chromosphere in the sebaceous gland, which is the target for infrared lasers. Selectively, it produces a dermal injury zone where sebaceous glands are located and therefore arrest the over production of sebum8.
1450 nm diode laser
The 1450 nm diode laser affects the pilosebaceous apparatus through peak thermal heating of the upper- to mid-dermis to a depth of 500 μm and causes thermal coagulation21. An infrared 1450 nm diode laser accompanying a dynamic cooling device reduces sebaceous gland activity and inflammation of acne lesions safely and effectively with fluences as high as 14 J/cm2.22 A study showed 76.1% lesion reduction from baseline was sustained on 20 patients 12 months after the final laser session. Therefore, the 1450 nm diode laser could provide a long-term remission in acne and sebum production23.
In contrast, in a split-face trial on 38 participants, one side of the face was randomly selected while the other side served as a within-patient control. A Candela 1450 nm Smoothbeam laser (Wayland, MA) was used with a double-pass technique, 6 mm spot size, 210 ms pulse duration and fluence of 8 or 9 J/cm2. Three treatments were performed 1 month apart. On average, within participants, the lesion count and acne grade reduced on both sides of the face by the same amount. Also, both remained similar 12 months after the last treatment24.
1540 nm erbium glass laser
In a study by Boineau D et al, they point to the efficacy of the 1540 nm erbium glass laser in treating acne25. In 2011, Isarría and colleagues treated 20 patients with acne and scarring. Each one achieved good results with four sessions with a 1-month interval between sessions. Active acne improved in 85% of cases, and a very large improvement was witnessed in 45% of cases. Pore size was improved in 75% of patients. Sebum secretion decreased in 80% of cases26.
Intense pulsed light
Many studies have used intense pulse light (IPL) sources to treat acne27-29. In one study, 180 randomised subjects with mild to moderate inflammatory and comedonal acne received vacuum and IPL, IPL alone, and sebium H2O Micellar Solution. The result supports the efficacy of IPL especially when combined with vacuum for comedonal acne29. The 530 nm IPL significantly reduces inflammatory lesions by its anti-TN-α effect and independent of IL-10 up-regulation30. Also, TGF-β1/Smad3 signaling is upregulated in perilesional skin with mild-to-moderate inflammatory acne vulgaris31.
Radiofrequency
Radiofrequency (RF) acts by reducing perifollicular inflammation. A combined RF and IPL treatment has been used to treat acne. In a study by Prieto et al, 4 weeks with twice-weekly sessions provided a 47% reduction of mean acne lesion counts in 32 patients32. Also, a monopolar radiofrequency device showed a reduction of more than 75% in inflammatory acne lesions after one treatment session in more than 90% of patients in a study conducted on 22 patients33.
Photodynamic therapy
During photodynamic therapy (PDT), aminolevulinic acid (ALA) is taken up by the pilosebaceous units. It is metabolised to protoporphyrin IX which when photoactivated converts to cytotoxic singlet oxygen and free radicals. This not only damages the pilosebaceous unit, but also causes the death of P. acnes34.
PDT requires three factors, a photosensitiser, light, and oxygen. The commonly used photosensitisers are (ALA) or methylaminolevilunate (MAL), the recent ones are indocyanine green (ICG) and indole-3-acetic acid. Arc lamps, light emitting diodes, IPL (filtered xenon flashlamps) filtered incandescent or fluorescent lamps, lasers, and sunlight are used as sources of light35.
In 2013, Ma et al suggested a low-dose (5%)topical ALA-PDT regimen, 1 hour incubation and red light source of 3 treatment sessions as the optimal schedule modality for different severities of acne vulgaris. Effective rate overall and of grade II, III and IV were 82.1%, 71.6%, 79.6% and 88.2%, respectively. Eight weeks after the treatment completion, maximum efficacy was obtained. Severe cystic acne of grade IV shows superior efficacy with mild side effects36.
Post-acne scar treatment with laser and light-based therapies
Recently, laser skin modalities for acne scarring have been primarily centred on laser resurfacing with erbium- doped yttrium aluminum garnet (Er:YAG) and carbon dioxide (CO2) lasers. Although these lasers have proven effective in improving scar appearance via collagen remodelling, they have been associated with extended recovery periods, prolonged erythema, hypo- and hyper pigmentation, and in rare cases, induction of additional scarring37-39.
Ablative laser skin resurfacing
Carbon dioxide laser
CO2 laser remains the gold standard technology for the most dramatic improvement in scars. Producing a wavelength of 10600 nm, the CO2 laser penetrates approximately 30 μm into the skin by absorption and vaporisation of water-containing tissue40. Sixty subjects (50 females, 10 males, skin types I-V, mean age 38 years) with moderate to severe atrophic facial scars received resurfacing with a high-energy pulsed CO2 laser. Clinical assessments and blinded histologic analyses of skin biopsies of treated scars were performed independently at 1, 6, 12, and 18 months. Significant clinical immediate and prolonged improvements were revealed in texture, skin tone, and appearance of CO2 laser-irradiated scars in all patients. Average scores of clinical improvement were 2.22 (69%) at 1 month, 2.1 (67%) at 6 months, 2.37 (73%) at 12 months, and 2.5 (75%) at 18 months. Collagenesis and dermal remodelling were observed histologically on examination of biopsied tissue up to 18 months after session41. Also, in another study, 24 subjects received forearm and facial treatments and these were well-tolerated; 83% of subjects exhibited moderate or better overall improvement42.
Qian et al conducted a study with 31 patients (11 women, 20 men, skin types III-IV) with facial acne scarring and treated them with three sequential fractional sessions over a 6-month period. Outcome and global improvement was evaluated blindly with before and after photographs by two physicians 3 and 12 months after the final sessions. Excellent improvement in scars presented in 12.9% of the patients, while 38.71% noted good to fair results. The clinical response at the 12-month follow-up visit tended to be better than at the 3-month follow-up visit, but was not statistically significant43.
This high-energy pulsed and cool-scanned fractional ablative CO2 laser system is safe and effective for facial atrophic acne scarring. Scar improvement was noted in the majority of patients with minimal discomfort, minimal downtime, and continued improvement43. A study conducted on 64 patients with moderate to severe facial acne scars of four sessions of either a Q-switched 1064 nm Nd:YAG or CO2 laser at a 1 month interval supports this further. The fractional CO2 laser showed significant effect on the improvement of atrophic acne scars, compared with Q-Switched 1064-nm Nd:YAG laser44.
In 2013, Mohammed developed a new pinpoint irradiation technique using a CO2 laser for treating ice pick acne scars. An open label pilot study conducted on 60 patients with ice pick acne scars revealed excellent improvement results, which were non-significantly different from the fractional laser45. This was also confirmed by Schweiger and Sundick46; 90% of 37 patients treated with IPL in combination with fractional CO2 laser significantly improved and 80% showed excellent response to inflammatory lesions and atrophic scars47.
Erbium yttrium-aluminum-garnet laser
Multiple passes with this laser are necessary to ablate to a similar depth as one pass of the CO2 laser, and because the Er:YAG effects are photomechanical instead of photothermal (like the CO2), intraoperative haemostasis is difficult to achieve40, 48-49.
Therefore, the short-pulsed Er:YAG laser is limited in its use for moderate-to-severe acne scars. Hybrid Er:YAG/CO2 laser systems are capable of delivering both CO2 energy for coagulation and Er:YAG energy for fine tissue ablation. The dual mode Er:YAG combines short pulses (for ablation) with longer pulses (for coagulation)50.
These lasers have been shown to produce deeper tissue vapourisation, as well as greater control of haemostasis, and collagen contraction. Overall clinical improvement was achieved in more than 50% of subjects with milder photodamage and scarring (Glogau classes I and II)51-52.
Non-ablative laser skin resurfacing
Recently, focus has shifted towards non-ablative technologies that deliver either laser, light based, or radiofrequency energies to the skin.
Pulsed dye laser
Used mainly for the treatment of hypertrophic scars. It has been hypothesised that the selective heating of dermal vessels leads to release of endothelial-derived growth factors and cytokines that up-regulate fibroblasts in treated skin, thereby resulting in neocollagenesis53.
Mid-infrared lasers
Laser systems located in the mid infrared portion of the electromagnetic spectrum, including the 1320 nm Nd:YAG, 1450 nm diode, and 1540 Er:Glass lasers, possess optimal wavelengths for water-based non-ablative skin remodelling. The 1450 nm diode laser in participants with Fitzpatrick skin types IV to VI was effective54-56. The latest generation of the 1320 nm Nd:YAG laser delivers energies ranging between 28–38 J/cm2 with a pulse duration of 350 µs through a 10 mm spot size hand-piece. Treatments are usually performed every month for a series of at least three sessions57-58.
Twenty patients (skin phototypes I-V) with mild to moderate atrophic facial acne scars randomly received three successive monthly treatments with a long-pulsed 1320 nm Nd:YAG laser on one facial half and a long-pulsed 1450 nm diode laser on the contralateral facial half. They were evaluated histologically and clinically and showed mild to moderate clinical improvement at 1, 3, 6, and 12 months postoperatively58.
Conclusion
Energy-based treatment options for acne and acne scars can be an alternative to medical modalities for non responders, those who have moderate or severe acne and are concerned about oral medications owing to potential adverse effects, or be used in combination with a topical medication. Devices targeting P. acnes, causing selective damage to the sebaceous gland and decrease sebum production are short-lived and require continued follow-up treatments; but result in long-term acne clearance. The results after treatment of acne scars will disappoint patients who desire dramatic improvement in a short period of time. The goal of any treatment in acne scars is not total cure or perfection; rather it is making scars less visible. Selection of appropriate technique requires that patient factors as well as the risks and benefits of the procedure be weighed.