Francesco P. Bernardini and Gabriela Casabona unveil a treatment algorithm dedicated to the treatment of the infraorbital region to improve results and minimise complications

email: [email protected]
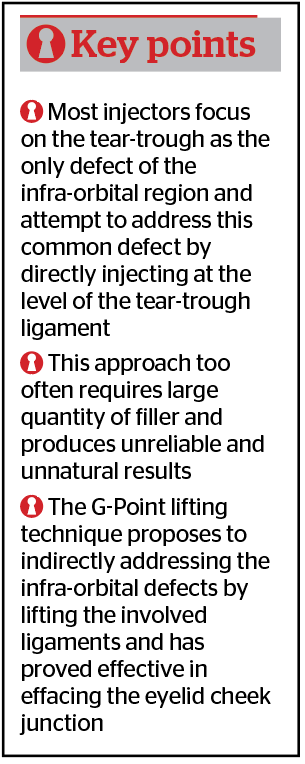
To improve the periocular region with fillers, injectors have traditionally focused mainly on treating the tear trough defect, as if this was the only goal of infraorbital treatments. Up to now, the most popular treatment to address the periocular region consists of a direct tear trough injection, using either a needle or cannula. However, this direct, ‘fill-the-hole’ approach is flawed by unreliable results and by risks of unsightly complications. For this reason, the authors have developed an anatomical approach, which has brought us to recognise a specific anatomical area, defined as the aesthetic ‘G-Point’ that takes advantage of the line of ligaments, the surface volume coefficient, and the G-prime of fillers to allow the injector to address the entire infra-orbital region while reducing the number of direct filler injections in the tear trough. In a recently published series of 306 patients, the authors achieved reliably improved results with minimised complications1.
Relevant anatomy of the infra-orbital region
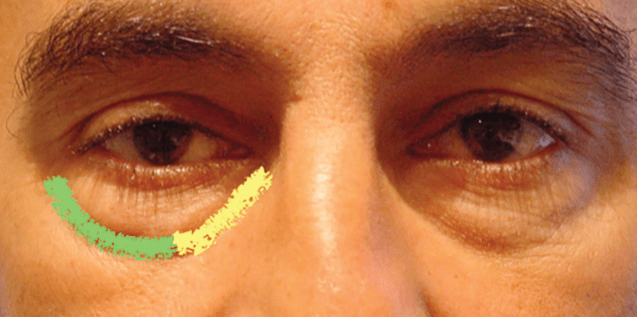
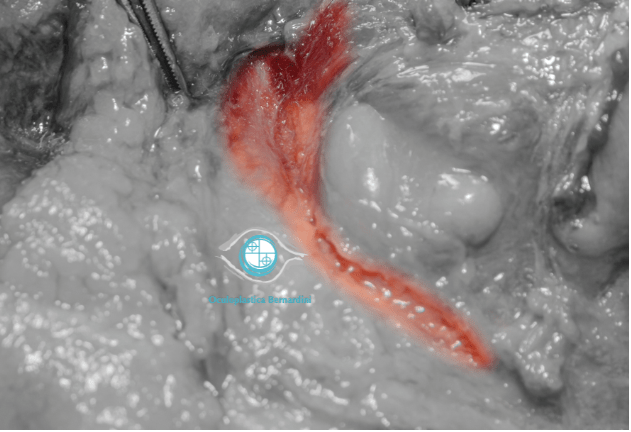
As anywhere else in the face, knowledge of the anatomy of the infraorbital region is key to understanding the extent of the clinically visible defect and the underlying structures involved in order to achieve reliable results. As evident from Figure 1, the so-called ‘tear-trough’ represents solely 1/3 of the infra-orbital hollow; it is clear that limiting our efforts to this defect only, significantly reduces the chances of achieving a complete aesthetic restoration. Also, the anatomical area depicted in Figure 2 demonstrates the relevance of the orbital retaining (ORL) and tear-trough ligaments (TTL) as two relatively wide structures tightly attached to the anterior face of the maxilla that separate the sub orbicularis oculi fat (SOOF) from the overlying infra-orbital fat (IOF). The surgical experience showed that ‘lifting’ of these two ligaments requires complete sharp dissection. This explains why attempts to elevate the ligaments by means of direct filler injection is difficult if not impossible without injecting too much product. In fact, direct injection with a needle on the periosteum of the tear trough defect as advocated by many injectors may push the filler on each side of the ligament, accentuating the same defect and predisposing to potential complications.
Defining the goals of the treatment
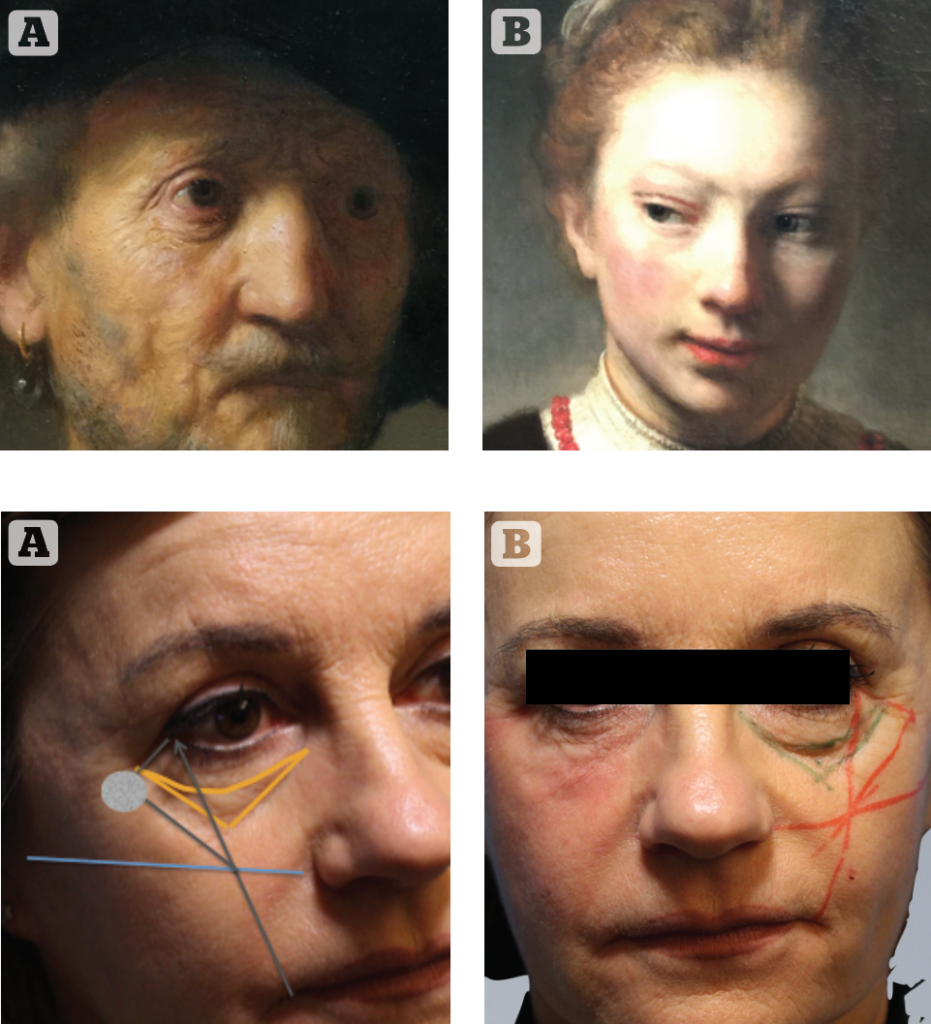
As a reminder of how a young infra-orbital region should be and how it changes during ageing, we don’t need to study our literature, as Rembrandt in the 1600s depicted very well the ageing of the infra-orbital region with its volume defects including bags and orbital-malar hollow, skin laxity and eyelid positional changes. Rembrandt also highlighted the natural youthful appearance of the periocular region, with an almond-shaped eyelid fissure, a single convexity between the eyelid/cheek junction with a short eyelid and tight eyelid skin (Figure 4). When examining a potential candidate for non-invasive treatment, we routinely dedicate an appropriate amount of time to diagnosing the ‘defect’ at hand and henceforth establishing a treatment plan, keeping in mind what our goals are in each specific patient in order to restore a youthful eyelid/cheek junction. Based on these findings, instead of considering the void of the tear trough as the only goal of filler treatment, we personalise the treatment plan, including the choice of the right products and the amount of filler necessary to achieve the result. With each patient, we focus on the evaluation of the following findings, using a flow chart with a scale from 1 to 4:
- 1) extension of the orbito-malar hollow (medial, lateral, central or complete)
- 2) presence of malar atrophy and determination of the fat compartment implicated (deep medial/lateral, SOOF, infra-orbital, middle)
- 3) presence of intra-orbital fat prolapse (eyelid bags, medial, central or lateral)
- 4) the presence of eyelid skin laxity
- 5) presence of dark circles
- 6) presence of naso-labial fold.
Introducing the G-Point
As surgeons, we have come to the understanding that a gentle pull from the lateral orbicularis provided significant improvement to the main defects of the entire infra-orbital region. We are aware that an almost complete correction of infra-orbital hollowing, eyelid bags, skin laxity and eyelid position can be achieved by means of a gentle lateral pull of the orbicularis muscle. As injectors, we have come to understand that this very same lateral lift proved effective in medical lifting, provided we take advantage of the different G-prime of fillers and we have come to adopt the very same point in both circumstances. We have defined this special point, demonstrated in Figure 5, as the ‘aesthetic G-Point’ because it combines a strategic anatomical area with the filler’s G-prime.
Treatment: algorithm planning and injection technique
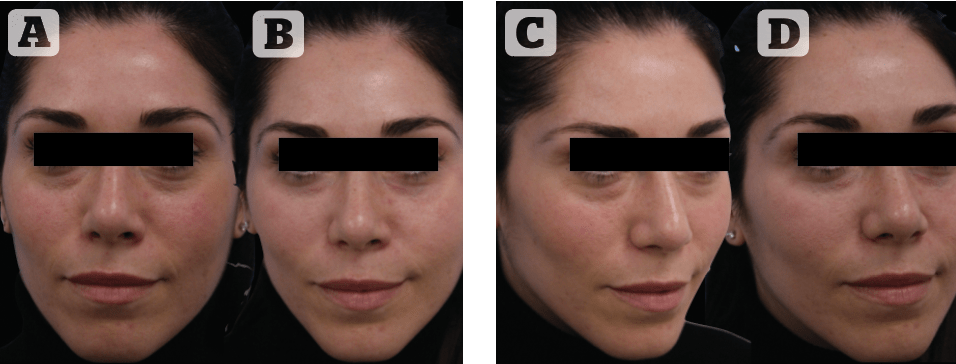
A retrospective study of the electronic medical records of a consecutive series of 163 patients who underwent infraorbital treatment using the ‘G-Point Lift’ from 2017-2018 was conducted in the private practice of the senior author (FPB). Macroboluses (.1 cc) of high G-prime filler, alternatively RHA4 or UltraDeep (Teoxane) were used initially using a high G-prime filler injected deeply at the ‘G-Point’ to provide a lifting effect and subsequently at the apex of the V-deformity of the lower eyelid to provide central support. Subsequently, micro boluses (.02–.03) of a dedicated low G-prime filler, namely Redensity II (Teoxane), were injected along the entire lower eyelid delivered in a ‘bridging’ technique. The immediate effect of the treatment is shown in Figure 6, that highlights the differences between the treated and untreated sides using the G-Point Lift. Results were determined by objective analysis, comparing pre- and post-procedure photos taken 1 month after the filler injection, using a four-point grading scale, where 0* = worsened, 1* = unchanged, 2* = mildly improved, and 4* = greatly improved, and by a subjective, anonymous satisfaction questionnaire delivered to the patients by non-medical assistants at the last follow-up visit, using a similar four-point grading scale.
Results
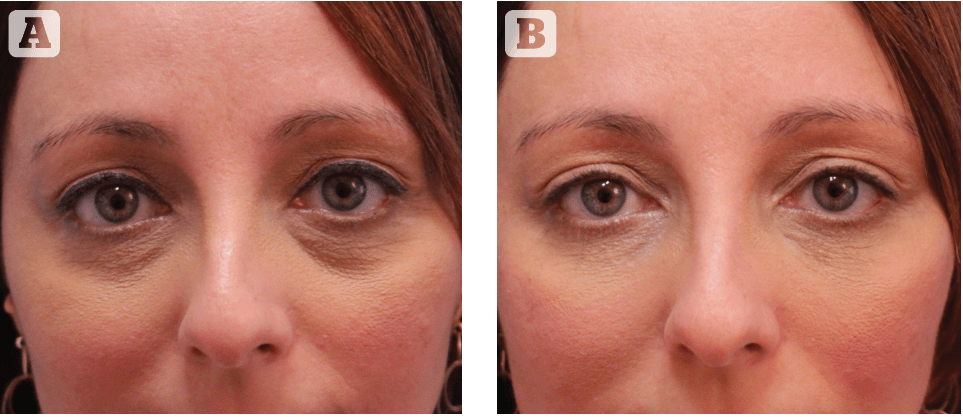
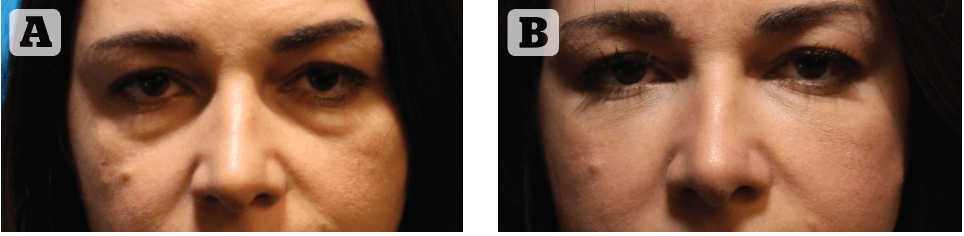
All patients were followed up for a minimum of 6 months following a ‘G-Point Lift’ treatment (mean 7.2 months). Objectively, all patients (100%) showed improvement (graded 3* or 4*). Patient satisfaction was recorded in all patients and the majority (73%) reported a great improvement (4*), 22.7 % were mildly improved, and two patients (1.23%) felt they were unchanged. Dissatisfied patients requiring hyaluronidase numbered only 5 (3%); reasons for been not satisfied included visible lumpiness at rest (2 patients) and visible lumpiness while smiling (3 patients). Patient satisfaction was recorded anonymously. These results are in accordance with what we have previously reported where the improvement 6 months after the procedure was excellent (>75% change) in 88.2% (n = 270) and good (51%–75% change) in 11.8% (n = 36) cases when rated by the treating physician; and was excellent in 81.4% (n = 249), good in 6.5% (n = 20) , fair in 11.8% (n = 36), and in one case little to no improvement was reported when rated by the patient1. Paradigmatic examples of the long-term results are demonstrated in Figures 7–9.
Discussion
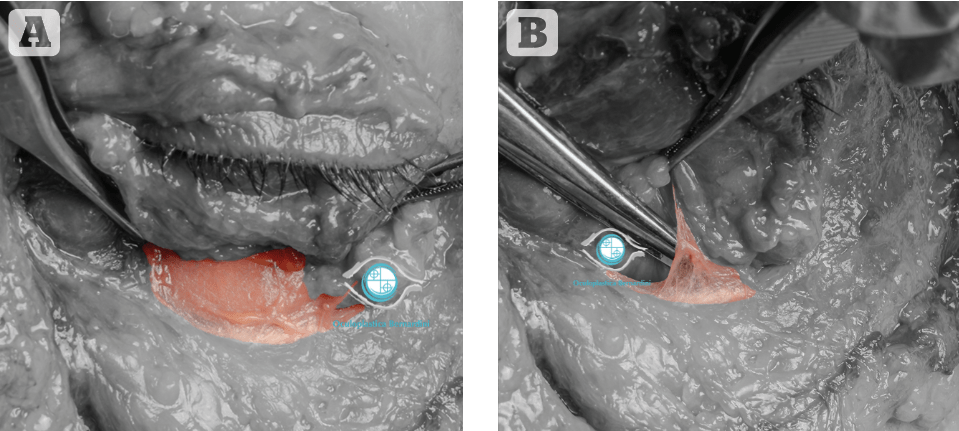
The effectiveness of the G-Point is explained by its anatomy: the G-Point lies in the lateral most part of the infra-orbital region, supero-lateral to the ORL. The ORL expands laterally to the lateral canthal region to form the lateral orbital thickening (LOT), while inferior to the ORL, the zygomatic-cutaneous ligament (ZCL) runs transversely across the malar region. The ZCL (inferiorly) and the ORL (superiorly) form the boundaries of the sub-orbicularis oculi fat (SOOF) and of the fat within the pre-zygomatic space, which is located deep to the SOOF. Both ligaments (ORL and ZCL) are anchored to the periosteum deep to the orbicularis oculi muscle (OOM) and lifting their periosteal insertion by means of direct injection is almost impossible without the release of this attachment; however, their dermal connections, visible on the skin surface, can be more easily stretched. We believe that a ‘G-Point’ injection is effective because of its anatomical location posterior and lateral to the line of ligaments, a position where the dermal adhesion of the ligament can be more easily stretched2. Injecting a macro-bolus of a high G-prime filler provides effective stretching of the dermal adhesion of the ORL and ZCL. The G-Point lift technique provided in our delivers ‘surgical’ results using a non-invasive approach. The same concept is applied to lower blepharoplasty in the authors’ practice; as surgeons, complete lower eyelid rejuvenation is achieved by combining orbicularis suspension performed at the ‘G-Point’ with central eyelid support provided by fat transposition associated with skin tightening. This surgical concept can be applied to non-invasive treatment of the lower eyelid, taking advantage of different filler rheology features, mainly their G-prime. The surgical habit of pre-operative preparatory markings was also applied to our non-invasive treatments; combining one drawing with another has confirmed the existence of the G-Point as a common specific point of maximal lifting effect, which maximises the effect of our surgical and non-surgical approaches equally. As injectors, a strong G-prime filler, delivered in macro-boluses of 0.1 cc used at the ‘G-Point’ achieves an eyelid lifting effect; when placed centrally, it provided similar eyelid support as that provided by surgical fat transposition. A low G-prime filler, delivered in micro-boluses of 0.02 cc, provides smoothing of the transitions at the medial eyelid and also skin tightening. As both surgeons and injectors, we have recognised the existence of common distinct anatomical point with powerful indirect effects, which makes the treatment more effective, simpler, and more reproducible and requires less ‘direct’ treatment. A stronger lift can be achieved by injecting at the ‘G Point’, whilst simultaneously improving the tear trough indirectly, thus requiring a much lower volume of direct tear trough filler injection.
Conclusions
In summary, by de-focusing our attention from the tear trough and applying a surgical approach to aesthetic medicine offers more natural and complete results while at the same time minimizing the risk of undesired side effects and complications.
Declaration of interest None
Figures 1–9 © Dr Bernardini
References
- Casabona G, Bernardini FP et al. How to best utilize the line of ligaments and the surface volume coefficient in facial soft tissue filler injections . J Cosmet Dermatol. 2019;00:1–9
- Casabona G, Frank K, Koban KC, et al. Lifting vs volumizing-The difference in facial minimally invasive procedures when re- specting the line of ligaments. J Cosmet Dermatol. 2019;18(5): 1237-1243.






