Aleksandar Godic reviews the benefits of using autologous adipose-derived stem cells in regenerative medicine.
Advanced age in humans is considered to be the greatest risk factor for a range of diseases, including cancer, Alzheimer’s disease, cardiovascular diseases, atherosclerosis, and metabolic syndrome, to name but a few. There exists the possibility that targeted approaches to anti-ageing will delay the onset of many pathologies that contribute to morbidity in the elderly, and will, therefore, achieve longer life expectancy or at least a healthier and more comfortable ageing1.
Ageing is the result of two overlapping processes, ‘intrinsic’ and ‘extrinsic’ ageing. ‘Intrinsic’ structural changes occur as a consequence of physiological ageing and are genetically determined2,3. The rate of ageing is significantly varied among different individuals and even among different anatomical sites in a single individual. Many theories have tried to explain the ageing process, but the most plausible of these concentrate on DNA damage and the concomitant repair process, which induce genome-wide epigenetic changes leading to cell senescence, loss of proper cell function, and genomic aberrations4. The signals from DNA-breaks lead to three responses regarding cell fate: transient cell cycle arrest (repair), stable cell cycle arrest (senescence), or cell death (apoptosis). Intrinsic (genetically determined or chronological) and extrinsic (UV- and toxic exposure-mediated) ageing processes overlap and are strongly related to increased generation of free radicals in cells, tissues, and organs. The underlying mechanism of both processes is increased oxidative stress, which is probably the single most harmful contributor to ageing, leading to loss of cells and the extracellular matrix5.
Manifestations of ageing
The clinical manifestations of intrinsic ageing reflect the balance between the severity of tissue and organ damage and their regenerative abilities. All proliferating and terminally differentiated cells are susceptible to harmful events leading to intrinsic ageing6.
The signs of ageing generally start early. By 40 years of age, most organs, tissues, and cells gradually become less efficient. The skin becomes thin, transparent, less elastic, and more lined and wrinkled. There is a loss of underlying fat on the face leading to hollowed cheeks and eye sockets. It is normal for hair to gradually thin on the scalp, pubic area, and armpits. As melanocytes decline in number, grey hair growth increases. Nail plates gradually thin7. By age 80, there are visible changes in posture due to compression of joints, spinal bones, and spinal discs. Regarding hearing, high-frequency sounds become harder to hear. Many elderly people develop presbyopia (the lenses in the eyes become less flexible) and a need for reading glasses. As we age, we will sleep less and not as deep compared to when we were younger. As we age, our bones become less dense and weaker. There is also more body fat and less muscle mass due to hormone changes. Problems with memory are normal and common. An elderly individual does not remember names as well as when they were young and has diminished short-term memory. The heart becomes less efficient and needs to overcome bigger resistanc
e as it ages and consequently starts to fail. The lungs supply less oxygen over time. The kidneys decline in function and un-cleared metabolites from medicines and metabolism build-up and cause toxicity. In men, sexual dysfunction is common, and women undergo a number of menopausal changes linked to lower estrogen production. In addition, an inactive lifestyle and unhealthy diet increase the risk of chronic diseases, such as coronary artery disease, osteoarthritis, high blood pressure, obesity, osteoporosis, type 2 diabetes, and cancer.
Stem cells
Induced pluripotent stem cells (iPSC) are derived from modified differentiated adult somatic cells and have the same properties as ESC. They are more acceptable since they are not derived from human embryos but involve major genetic modifications in in vitro conditions before they can be used for research and clinical applications10,11.
Adipose-derived stem cells (ASC)
Autologous adult stem cells are immunocompatible, and there are no ethical concerns related to their use. Multipotent mesenchymal stem cells (MSC), which have similar characteristics to bone marrow derived MSC, are nonhematopoietic cells, which originate from mesoderm and are present in various postnatal organs and connective tissues, including: trabecular bone12, periosteum13, synovial membrane14, skeletal muscle15, skin16, pericytes17, peripheral blood18, deciduous teeth19, periodontal ligament20, and umbilical cord21,22. Adult stem cells derived from these tissues would require ex vivo expansion or manipulation before they could be used clinically, since their quantity in the mentioned tissues is low. It has been found that multipotent stem cells within adipose tissue, termed adipose-derived stem cells23, are one of the most promising stem cell populations identified thus far, since human adipose tissue can be easily harvested through liposuction with only minimal patient discomfort. Therefore, the use of autologous ASC has been shown to be safe and efficacious in preclinical and clinical studies24,25. To date, a number of scientific papers on ASC biology and their use in regenerative medicine have been published, and their efficacy has been determined in several clinical trials24,25.
Localization and cellular characteristics of ASC
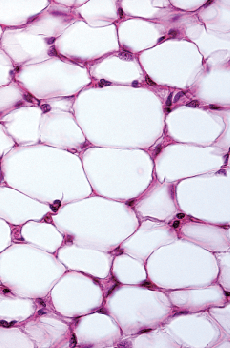
Adipose tissue is composed mainly of adipocytes (fat cells), which are clustered into fat lobules26. It consists of mature adipocytes (more than 90% of the tissue volume), and a stromal vascular fraction (SVF). Stromal vascular fraction is composed of pre-adipocytes, fibroblasts, vascular smooth muscle cells, endothelial cells, resident monocytes/macrophages, lymphocytes, and ASC27,28. Characteristics of ASC differ according to the location of the harvested adipose tissue. Most resistant to apoptosis are ASC harvested from superficial abdominal regions, followed by those harvested from medial thigh, trochanteric, and superficial deep abdominal depots29. The density of stem cell varies among different locations and types. They are more abundant in the subcutaneous compartment of white adipose tissue compared to visceral fat30. Likewise, it has been reported that ASC have been found within the brown adipose tissue, which possess skeletal myogenic differentiation potential31.
Freshly isolated stromal vascular cells (SVF) are a heterogeneous cell population that includes ASC, endothelial cells, vascular smooth muscle cells, pericytes, and hematopoietic cells in uncultured conditions32. Freshly isolated SVF and those after a few divisions express higher levels of CD117 (c-kit), human leukocyte antigen DR (HLA-DR), and stem cell-associated markers (e.g. CD34), as well as lower levels of stromal cell markers22,32–48. As they proliferate, they lose CD34 surface antigens44. Adipose-derived stem cells, which express CD34+ have a greater proliferative capacity, while those which do not express CD34- are more plastic33,49.
Adipose-derived stem cells share many cell surface markers with pericytes and bone marrow-MSC33. It has been published that ASC are most likely located within the perivascular tissue since they express pericyte surface antigens50,51. ASC are capable of dividing, self-renewal, and proliferation due to their telomerase activity, which is diminished as they age52. They do not exhibit immunosuppressive properties because they do not express HLA-DR antigens on their cell surfaces53.
The role of ASC in regenerative medicine
Previous studies have suggested that ASC exhibit their beneficial effects (angiogenesis, anti-inflammation, and anti-apoptosis) mostly through secreted cytokines and growth factors rather than their differentiation into various cell types54,55. The ASC cytokines and growth factors have the potential to be used in cell-based treatments in regenerative medicine due to their promotion of fibroblast proliferation and the differentiation of ASC to fibroblast. They also play a role in collagen secretion. In addition, they inhibit tyrosinase and consequently cause whitening of the skin. A number of papers have described the secretory factors of pre-adipocytes, ASC, or adipose tissue56,57. Cultured ASC (after a few divisions), secrete adiponectin, angiotensin, basic fibroblast growth factor (bFGF), cathepsin D, CXCL12, granulocyte-macrophage colony-stimulating factor (GCSF), hepatocyte growth factor (HGF), insulin-like growth factor (IGF)-1, interleukins 6–8 and 11, pentraxin, pregnancy zone protein, retinol-binding protein, transforming growth factor β (TGF-β), tumor necrosis factor α (TNF-α), and vascular endothelial growth factor (VEGF)56, 57, 58.
Proliferation capacity of ASC
Previous reports have shown that ASC double in number between 40 to 120 hours depending on donor age, type of adipose tissue (white or brown), location (subcutaneous or visceral), the harvesting procedure, and culture conditions23, 43, 59, 60. The proliferation capacity of ASC is at its greatest in young individuals and diminishes as we age. In addition, ASC also gradually lose proliferative capacity in in vitro conditions60. Senescence of ASC is similar to that witnessed in bone marrow-derived MSC59. Adipose-derived stem cells remain stable as they proliferate in culture and do not change their diploid karyotype61. Their proliferation can be stimulated by various growth factors, among which fibroblast growth factor 2 (FGF-2) is most important and required for their self-renewal62, 63, 64. The proliferation of ASC can also be stimulated by platelet-derived growth factor (PDGF) and oncostatin M65, 66. ASC proliferation can also be stimulated by growth factors supplemented by thrombin-activated platelet-rich plasma67, human platelet lysate68, and human thrombin69.
Differentiation potential of ASC

Intravenous administration of ASC in animal models on brain ischemia or hemorrhage demonstrated functional and histological improvement88, 89. In addition, recent studies have revealed a beneficial effect of intravenously administered ASC in animals with a spinal cord injury since they migrated and partially differentiated into neurons and oligodendrocytes, and restored locomotor function90.
Last but not least, it has been demonstrated that ASC can differentiate into endoderm lineage cells. It has been published that ASC have the potential to differentiate into hepatocytes91, 92, which raises the possibility for them to be used to reduce liver inflammation and treat liver fibrosis. In addition to hepatic differentiation, ASC under in vitro conditions can differentiate in insulin, glucagon, and somatostatin producing cells93, 94.
Discussion
Apoptosis and cellular senescence (damaged cells that have lost the ability to divide) are considered to be important factors in ageing and age-related diseases. Dead cells are replaced by new in the process of regeneration. They originate from stem cells, although their proliferating/differentiating capacity depends on the age of the donor; as we age, the proliferation capacity of stem cells diminishes and leads to senescence.
Rejuvenation and ageing deceleration could be achieved by elimination of senescent cells, but their epigenetic reprogramming is not yet fully understood. Another approach to reset ‘the ageing-clock’ and to improve chronological ageing is to replace stem cells either through intravenous or local administration95.
Adult adipose-derived stem cells seem to be a powerful tool in regenerative medicine since they can differentiate into all three embryonic tissues. It has been published that the number of isolated stem cells per gram of processed adipose tissue is greater than that derived from bone marrow, which is another advantage for use in regenerative medicine60. Routinely, 1 x 107 adipose stromal/stem cells have been isolated from 300 ml of lipoaspirate, with greater than 95% purity96. The average frequency of ASC in processed lipoaspirate is 2% of all nucleated cells97.
Adipose-derived stem cells can be harvested by minimal abdominal liposuction performed with local anaesthesia, and processed by medical devices, which ideally should be part of closed, sterile, and standardized systems, to avoid toxicity, pyrogenicity, hemolysis, sensitization and genotoxicity, as well as to maintain their viability.
Adipose-derived stem cells are currently used in reconstructive and aesthetic medicine. They are used as a heterogenous cell suspension of SVF in breast augmentation and craniofacial soft tissue and bone restoration by their local application into the breast and the face. They can also be used in patients with severe heart failure by injecting them in coronary arteries, and in patients with musculoskeletal disorders by injecting into affected joints, although those treatments are not standardized and widely accepted. In addition, there are many clinical trials on their use in various conditions, such as peripheral vascular diseases, fistulas, diabetes mellitus, liver cirrhosis, lipodystrophy, spinal cord injury, faecal incontinence, degenerative arthritis, radiation ulcers, and graft-versus-host disease (GVHD)70. Last, but not least, the author believes that they can be successfully used in anti-ageing medicine to decelerate ageing.
As we age, our stem cells lose the ability to self-renew and to differentiate and consequently to replace aged cells with new ones (diminished regeneration). ASC communicate with surrounding cells by secreting cytokines and growth factors and differentiating into them. Their secreting cytokine profile is similar to the cytokines that are present in the local environment around them (e.g. bones, cartilage, tendons, muscles, skin) and as such maintain tissue regeneration.
Is has also been well reported, that ASC has beneficial effect on lipografts. The main side-effect of autologous lipotransfer is unpredictable graft resorption due to ischaemia and insufficient neoangiogenesis, which may ranges from 25%-80%. This is inconvenient because a number of procedures need to be performed before a satisfactory cosmetic outcome is achieved.
A review of the literature on autologous fat breast augmentation found 36 papers (1500 healthy women have been included, average follow up period was 16 months). The average breast volume gain was reported to range from 55%–82%. To overcome the problem of unpredictable results, autologous fat grafts have been enriched with ASC before transplantation. Four murine and three human studies on autologous lipotransfer have been found. ASC-enriched fat grafts (compared to non-enriched grafts) resulted in considerably improved fat graft survival (due to increased neovascularization and decreased inflammation) as well as quality (with minimal resorption rate), although too many ASC in grafts promoted graft necrosis, and the formation of vacuoles and fibrosis. It has been found in an murine model that 3 x 105 of ADS/ml of grafted fat has been shown to be the optimal concentration estimated by maximized desirable and minimized undesirable effects98.
Conclusion
Adult adipose-derived stem cells (ASC) seem to be a powerful tool in anti-aging and regenerative medicine since they can differentiate into all three embryonic tissues and secrete many cytokines and growth factors. Currently there are many clinical trials on their usage in various conditions, and results are promising. They can be harvested by minimal liposuction in autologous donors and administer locally or intravenously on the same day without previous genetic manipulation or their expansion in in vitro conditions. It has also been well established that number of adipose-derived stem cells per gram of processed adipose tissue is much greater than in bone marrow, which is another advantage in their usage.







