Rosacea is a common cutaneous condition, but one that is frequently overlooked. As a result of its multifarious nature (especially between ethnicities) and characteristic relapses and remissions, diagnosis is complex. Currently, clinicians are only identifying the advanced, more obvious forms of rosacea. In practice, however, milder states prevail, and their markers are soft — especially early on. Prevalence rates in the literature are controversial, and mirror this discrepancy. Although traditionally considered ‘the curse of the Celts’, a recent Irish study cited rosacea frequency at only 2%. This author, however, makes a compelling argument that these numbers are closer to 80%. Physicians must be encouraged to improve their rosacea diagnostic capabilities, by actively searching for discrete clues that precede the unfortunate advanced states. In this way, treatment will be proactive rather than reactive. With novel insight into disease pathogenesis, therapeutic choices should remain holistic to optimally achieve skin health, while also incorporating these advancements.
Rosacea is a chronic dermatosis primarily affecting the convexities of the central face (cheeks, chin, nose, and central forehead), with remissions and exacerbations typifying the disease. Typologies encompass a range of combinations of such cutaneous signs as flushing, erythema, telangiectasia, oedema, papules, pustules, ocular lesions, and textural changes (large pores, sebaceous gland hyperplasia, and rhinophyma)1. The aetiology of rosacea has long been disputed, but current research has shifted the pathogenesis paradigm to inflammation with neurovascular dysregulation2.
Although deemed a common dermatologic condition, rosacea is shockingly overlooked3. Physicians often limit their diagnosis to advanced states, where numerous and easily recognised features are present with secondary sequelae. In practice, it is common that some rather than all of the signs appear in patients, and these are usually subtle — especially early on in the disease4.
April marked Rosacea Awareness Month, affording an opportune time to encourage clinicians to improve their diagnostic capabilities, by actively searching for discrete cues that precede the strawberry-like facies; a ruinous advanced form. A firm understanding of current rosacea aetiology will improve identification of these signs and promote early detection. In doing so, disease progression can be halted, thereby reducing the impending disfigurement, the need for multiple supplemental procedures, and costliness. Furthermore, treatment modalities that practitioners select should mimic the advancements in pathogenesis. The focus, however, must not be myopic and limited to rosacea symptom improvement. Rather, the underlying cause should be addressed. Today, the strawberry fields of rosacea don’t have to be forever.
Diagnosing rosacea throughout history
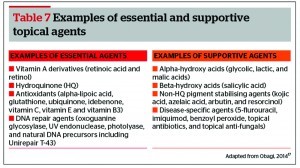
1) Acne rosacea illustration (Thomas Bateman, 1830). 2) Acne rosacea illustration (Ferdinand von Hebra, 1869). 3) Rosacea photograph (photogravure technique) (George Henry Fox, 1880)5
The heterogeneous signs and symptoms of rosacea appear in paintings as early as the 1400s, but their association with a disease state was not understood5.
As dermatology became established in the 19th century, rosacea was one of the first disorders to be identified. Physicians relied heavily on hand coloured illustrations in medical textbooks to aid in diagnosing diseases, and distinguishing one skin condition from another. The first rosacea drawing dates to the 1817 edition of On Cutaneous Diseases by Dr Robert Willan5. Oftentimes, rosacea images appeared alongside those of acne, but the features were exaggerated to differentiate the disease. A blue or purple tint was given to bumps and pimples, while telangiectasia was portrayed as cracks in the skin5. Furthermore, because no treatment options were available at that time, the depicted faces were sorrowful, among advanced and alarming disease.
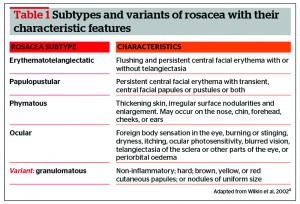
As the century progressed, so did the recognition of rosacea as being separate from acne, and with the introduction of photography, rosacea representation became more realistic5. In 2002, the ‘standard classification of rosacea’ was published by a consensus group, along with a grading system for the condition (Table 1)4. This provided clinicians with a standardised framework to better diagnose the disease. Through medical therapy and lifestyle changes, treatments now exist that allow patients to avoid the extremes known by sufferers in centuries past, and to improve their quality of life.
The underdiagnosis
Rosacea is a common dermatologic disorder, but one that is frequently overlooked3. The symptoms, signs and disease progression vary between patients and among ethnicities. To further complicate matters, rosacea may be in a state of temporary remission on patient evaluation.
Ruby-red skin peppered with spots and prominent blood vessels, all framing an engorged nose, typify the appearance. However, this generalised stigma is in fact a comparatively rare and advanced form of the disease. In practice, most patients have only mild symptoms, and some rather than all of the hallmark signs will be present4.
Despite its long-standing prevalence, little is known and agreed on when it comes to rosacea. The definition, aetiology, pathogenesis, diversity of clinical manifestations, and management all currently remain disputed. Furthermore, there exist no serologic or histologic markers. Rosacea may further be overlooked in non-Caucasian patients because of a low index of suspicion or atypical presentation because of skin pigmentation3, 6. It is no wonder then, that diagnosis is difficult for practitioners, and reserved for advanced, more classic, fair-skinned presentations.
However, physicians are not the only ones contributing to disease under-representation; patient factors must also be considered. Compellingly, 78% of Americans have no knowledge of rosacea, including how to recognise it or what to do about it7. Furthermore, mild or transient symptoms are rarely discussed with physicians, and may be mistaken for something else, such as sunburn3. Detection bias may also play a role, as women seek medical care more often than men8.
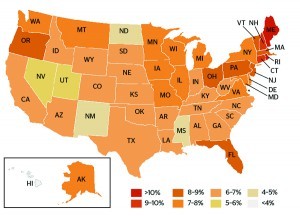
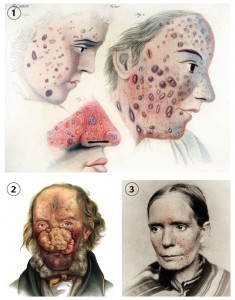
Figure 1 Estimated rosacea prevalence in US adult population, based on National Rosacea Society membership as a proportion of state populations over 18 years (adapted from National Rosacea Society, 201315)
The epidemiology
Epidemiologic data on rosacea is scarce and exceptionally controversial9. In the literature, prevalence rates range from 0.09% to 22%10. It is frequently referred to as ‘the curse of the Celts’, but a recent Irish study placed rosacea rates on the lower end of the spectrum, at just 2%11. The reported numbers are similar in Australia and Germany, where prevalence is 1.4% and 2% respectively11, 12. Conversely, a frequently referenced Swedish study revealed a rosacea rate of 10%, while in Estonia it is reported at 22%10, 13. Research from the US placed overall rosacea frequency at 9.6%, but the prevalence in Caucasian women alone was 16%14.
Amid such conflicting statistics, rosacea is still quoted as a disease of fair-skinned people of Irish, English, and German descent3, 15. In the US, rosacea concentrations remain highest in states with the largest concentrations of these ancestries: Maine, Rhode Island, New Hampshire and Connecticut (Figure 1)15.
Perhaps this inconsistency among epidemiology statistics is due to many of the same reasons why underdiagnosis occurs. Even the higher prevalence rates are likely flawed, and under-represented. Although rosacea is chronic, the outward manifestations are characterised by relapses and remissions. Most studies only examined the presence of signs and symptoms at the time of research. Therefore, at any given point, many rosacea sufferers are excluded because they are in temporary remission. Furthermore, skin with pigment has wonderful camouflage capabilities, allowing it to mask the vascular dysregulation associated with the disease14. Rosacea may have been present in these ethnicities, but not easily identified, and therefore its primary association with European ancestries is debatable.
The author’s experience
The author currently resides in Ireland and in her clinical practice, rosacea diagnostic rates are approximately 80%; a figure significantly higher than any formerly published. Most of her patients are of Celtic ancestry, with soft signs and symptoms previously overlooked. Frequently, their presenting complaint is not related to the rosacea, and this is an incidental diagnosis based on subtle markers.
As a global brand ambassador, she also teaches clinicians (dermatologists, plastic surgeons, aesthetic practitioners, family physicians, aestheticians, nurses) internationally about skincare advances. At the end of training, an exercise is performed whereby students are asked to create a topical treatment protocol suited to their skin. Interestingly, rosacea is seldom ever self‑diagnosed among these professionals during this task (roughly 20%). However, the author has witnessed frequency rates among these students of varying cultures and ethnicities, closer to those that she experiences in Ireland (70–80%). If clinicians are unable to diagnose themselves, then this further emphasises the likelihood that rosacea prevalence is grossly underestimated in the communities (medical and non‑medical) they serve.
Even more compelling, is that when she later returns to teach these same students advanced courses, they too remark that the latest diagnostic rates in their clinics closely resemble those that she suspects.
The aetiology
Rosacea is an inflammatory process, the specific cause of which is still unknown3. It appears to be heavily influenced by sebum, but genetics, hormonal fluctuations, and lifestyle all play contributing roles16. Interestingly, rosacea is less common among smokers because of its anti-inflammatory effect. However, should the patient quit cigarettes, rosacea rates rise to match those of non-smokers9.
Inflammation is the immune system’s defence against an insult to its integrity. Until relatively recently, inflammation (both acute and chronic) was not considered an important factor that required control. Now it is increasingly evident that inflammation is a destructive process in both diseased and disease-free skin. Cutaneous inflammation alters the permeability of skin, and weakens the epidermal barrier function17. This leads to sensitive skin, a common complaint among rosacea sufferers. As inflammation destroys elasticity, textural changes are common. Also influenced by the inflammatory cascade, extrinsic ageing and melanin production are intensified17. It is therefore not uncommon to witness accelerated ageing and non-specific discolouration among rosacea sufferers.
The cathelicidin pathway in particular is upregulated and hyper-reactive in rosacea, a cascade normally present in skin to recognise and neutralise invasion by microbial organisms2. This upregulation produces excess cathelicidin (LL-37), which induces vasodilation of superficial facial vasculature, inflammation, and vascular proliferation. Early rosacea candidates typically have a discretely pinkish hue, but with time and impending disease progression, this tone intensifies and becomes fixed, as the blood vessels reach permanent dilation. In some patients, temporary flares occur in response to established triggers, and this is owing to mast cell activation of certain types of cathelicidins (Table 2)18, 19.
The literature leads us to believe that sebum excretion rates and skin surface lipid composition are not altered in rosacea patients20, 21. However, these studies are limited, archaic and questionable. Sebum contributes to rosacea and is immunogenic. The characteristic enlarged pores and sebaceous gland hyperplasia of rosacea exemplify this4. Arguably, even if the lipid levels are maintained, it is possible that their composition is altered or that they are more proinflammatory. Furthermore, oil-associated comedones are not listed as a feature of rosacea, but rather one of acne. Comedones are, however, unquestionably widespread in rosacea, especially perinasally. This suggests concomitant acne, but the literature reports coexisting rosacea and acne rates of only 7%22. Seborrhoeic dermatitis, yet another disease propelled by excess sebum, is three-times more common in rosacea sufferers9. Furthermore, the facial distribution of rosacea (cheeks, chin, nose, and central forehead) coincides with the same anatomical location of sebaceous glands; another point favouring its contribution4, 16.
Oil glands are adnexal skin structures, and are remnants from when we were apes. The original purpose of these glands was to produce sebum to lubricate the hair follicle and repel water. As we evolved from this primitive form, we lost the excess hair of our ancestors, and retained the oil glands. Oil serves no purpose to the skin; it causes detriment and disease17. Specific to rosacea, oil is commonly trapped beneath accumulated dead surface keratinocytes. This leads to comedones, pustules and inflamed papular lesions. Clogged pores further yield a false sense of dryness17. Aiming to combat this sensation, the patient is drawn to using a moisturiser; an agent that inflames the rosacea. Topical steroids are also commonly used to reduce the sensation of burning and irritation induced by a disrupted barrier function. Paradoxically, these agents further weaken the barrier function, and suppress keratinocyte activity and maturation.
Moisturiser misuse
The misuse of skincare products is an important contributor to disease. Patients are ill-informed about topical agents suited to their skin type, and so frequently make unhealthy selections. Moisturisers are one of the most commonly found skincare products in any household. They are a widespread yet silent traitor. Through their flagrant mismarketing, it is suggested that moisturisers can remedy an abundance of skin complaints. Individuals are further drawn to their use by attractive packaging, alluring scents, and the comforting feel when applied.
However, it is the misuse of moisturisers that is injurious. Moisturisers are a necessity in a number of conditions, including genetically dry and sensitive skin (e.g. atopic dermatitis, xeroderma pigmentosum). These states require moisturisers regularly. This is because the skin in these patients has an inherently disturbed barrier function (water/lipid/protein balance), and so requires this artificial supplement. Likewise, when clients are undergoing anticipated reactions (redness, dryness, exfoliation) from strong therapeutic regimens (e.g. retinoic acid), a moisturiser is advocated to calm the skin from excessive irritation. This is only usually necessary during the initial phase, for as the reactions subside, so too should the need for a moisturiser. Certain environmental conditions (e.g. low humidity levels, cold temperatures) will also demand more frequent use of moisturisers, because the harsh environment will independently dry the skin. Furthermore, cosmetic procedures cause acute inflammation and dryness, which if not managed appropriately, will lead to chronic inflammation. To prevent this destructive process from occurring, moisturisers rich in anti‑inflammatory agents should be used temporarily after cosmetic procedures. These will calm the skin, and aid in healthy wound healing.
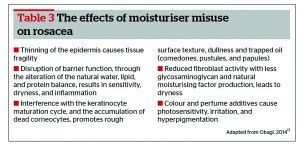
The adverse effects associated with moisturisers stem from blind and inappropriate use17. Moisturiser misuse leads to thinning of the epidermis (tissue fragility), an accumulation of dead surface keratinocytes (dullness, rough appearance, acneiform lesions), barrier dysfunction (sensitivity, dryness, inflammation), and reduced fibroblast activity including less natural moisturising factors (NMFs) and glycosaminoglycan (GAG) production (dryness)17. Furthermore, they often have colour or perfume additives, which are both irritating and photosensitising.
Moisturisers comprise water, lipid and protein, the proportion of which determines their weight and occlusiveness. Patients often begin by using a light water based lotion, and their dependence on the product occurs in as little as 3 weeks. The tight feeling they begin to experience on exiting the shower, and the need for immediate moisturiser reapplication signifies this. As cells become reliant on this artificial source of water, lipid, and protein, they become increasingly lazy, and in time, a heavier, more oil-based formulation is sourced.
Moisturiser misuse propels rosacea in a number of ways (Table 3). Their use must therefore be cautioned, and limited to the specific states described above. Agents that improve natural moisturisation from within the skin should instead be used.
Natural moisturisation
There are two specific functions enabling natural skin hydration17. It is necessary that both of these be intact if moisturisation is to be achieved. These properties are17:
- The dermis must host fibroblasts that are active and functioning appropriately. Fibroblast cells produce collagen, elastin, NMFs, and GAGs. The latter two are particularly important for hydration, acting like sponges within the dermis to attract water and saturate this layer
- The epidermis must fulfill its role in acting like a barrier. In doing so, it prevents the evaporation of trapped water from the dermis, essentially damming it. The key to a properly functioning epidermis with an intact barrier function is the correct proportion of water, lipid, and protein.
Moisturiser misuse induces sensitivity and dryness in skin. As an external source of water, lipid, and protein, moisturisers disrupt the natural balance within the epidermis. No longer able to perform its barrier role, allergens are able to penetrate the skin and cause sensitivity. Moisturisers further promote fibroblast indolence, because the skin is saturated artificially.
The hallmarks
Rosacea is a multifarious disease with presentations that fluctuate from patient to patient3, 4. Typically, rosacea skin has an overall oily appearance. Large pores owing to damaged elasticity accompany this. Sebaceous gland hyperplasia is often present, but frequently missed. Sebum may become trapped, leading to congested pores, and red, dome-shaped, papular lesions that are less pustular compared with acne, and more inflammatory in nature4. These often occur together in crops, and sometimes nodules may appear.
Interestingly, most rosacea sufferers remark that their skin is dry. In fact, it is not uncommon to see scaling, especially around the central face. This can be secondary to moisturiser misuse with resulting barrier disruption17. Alternatively seborrhoeic dermatitis, a common feature of rosacea, may be present9. Sensitivity, described as a ‘burning’ or ‘stinging’ sensation, is a common complaint, but this is because of irritation rather than the disease process.
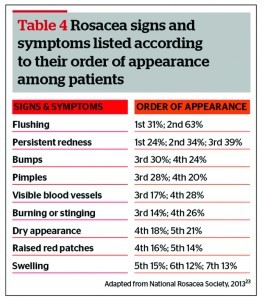
The first most commonly experienced among rosacea patients is ‘easy flushing’, but this is not always present (Table 4)23. Although flushing can occur early on, it usually signifies a more aggressive form of the disease. This is because the inflammation is triggering a systemic response with prominent neurovascular dysregulation2.
The colour of the skin will often initially appear pink and patchy, but this can be a subtle and transient marker3. Later, the generalised rubicund face will dominate. If present, the associated telangiectasia may be easily identified. In some cases, however, the skin will require stretching in order to reveal a deeper underlying mat of blood vessels. Non‑specific skin discolouration is common, but should a disease of melanocytes be concurrently present (e.g. melasma), the rosacea will envigor the condition17.
Ocular manifestations often occur, and their severity may not be proportional to those of the skin3, 4. A study from 1953 reported that ocular symptoms preceded dermatological findings in up to 20% of patients with rosacea24. These range from burning or itching, to signs of conjunctival hyperaemia and lid inflammation. Styes, chalazia, and corneal damage may also be present. Regrettably, only 4% of rosacea diagnoses are referred to an ophthalmologist9.
Associated oedema can be temporary or persistent3, 4. Transient, soft oedema may last for a number of days, and typically follows prolonged facial erythema or flushing. Solid facial oedema (persisting hard, non-pitting oedema) may also occur, but usually as a consequence of advanced disease.
Phymatous changes may be observed: patulous follicles, skin hypertrophy, irregular surface nodularities, and enlargement4. Rhinophyma is the most common presentation, but phymas can occur in other locations such as the chin, forehead, cheeks, and ears. Expressive follicles and telangiectases frequently overlie the phymatous area.
Yellowish–brown, hard nodules would suggest granulomatous rosacea, which is a rare variant, and represents only 10% of cases4. Characteristic lesions are less inflammatory, and sit on normal-appearing skin of the cheeks and periorificial regions.
Piecing together the clues
The key to managing rosacea is early detection, so as to avoid permanent textural and vascular transformation, necessitating ancillary procedures. The advanced, more classical form of rosacea is what clinicians are currently diagnosing. Their signs are obvious, and can be easily recognised from ‘across the room’. In practice, however, milder forms prevail. Their indicators are not as conspicuous, and require ‘up close’ scrutiny to arrive at the diagnosis. Furthermore, skin manipulation such as stretching is key.
It is worth remembering that some symptoms, such as flushing, are transient, and the disease may be in an inactive state. Bearing in mind the aetiology behind rosacea, there are many easily identified markers to aid in diagnosis. Even when the disease is in remission, a trail is left behind for the clinician to follow. The majority of these markers revolve around inflammation and oil; the primary crusaders leading the process of skin destruction. Such factors are particularly important to recall when attempting an early diagnosis, as the clues may be subtle.
In the author’s experience, the most frequently observed combination of early rosacea signs include:
- Oily skin with large poresSebaceous gland hyperplasia
- Feint erythema
- Telangiectasia
- Acneiform lesions.
These, however, may not consistently be present together. Some signs must be actively searched for. Sebaceous gland hyperplasia is a fitting example, and questioning the patient about specific lesions
that become aggravated and reoccur is helpful in pinpointing these.
Within the history, age can assist in identifying rosacea, and distinguishing it from acne. The vast majority (80%) of rosacea patients are at or above the age of 30 years9. Comparatively, acne is a disease of teenagers. Furthermore, rosacea is limited to the face, but the trunk and arms are often also affected in acne25.
Studies have reported rosacea prevalence rates three times higher in females3. This is debatable, and possibly owing to detection bias from presentation disparity8. Flushing and exacerbation by triggers may lead the physician to a diagnosis, but these are unreliable. Neurovascular dysregulation follows a spectrum of severity, and may only be mildly present. Furthermore, should the disease go undiagnosed for a long period of time, said symptoms are overlooked by the patient. Sensitivity and moisturiser use is also worth inquiring about, as they will play an important role when selecting an appropriate treatment protocol.
Healthy skin
When treating skin disease, physicians commonly have a blinkered approach, focusing on symptoms and their improvement. Rather, the underlying cause should be identified and addressed. Disease is not restricted to what we can see or feel; it affects all cells and layers within the skin. An holistic approach to treatment will therefore prove more successful and long-lasting.
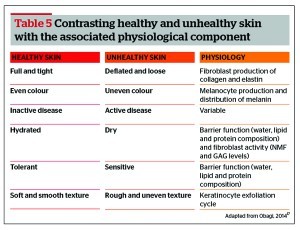
It is worth noting that healthy skin is not simply the absence of disease. Rather, this definition encompasses all cells and layers, ensuring that each is functioning correctly and harmoniously. Healthy skin also displays tolerance, hydration, fullness, tightness, even colour, and softness (Table 5)17. When disease is present, a number of these features may be altered simultaneously. In order to achieve optimum results, and restore overall skin heath, these should be treated concurrently.
Treatment
While there is no cure for rosacea, effective treatment options do exist and can be tailored to the symptoms and disease severity1, 16. An important preliminary measure is to educate patients about recognising and avoiding triggers (Table 2)3, 18. These vary between patients, but alcohol, spicy foods, extreme temperatures, and sun exposure are common contributors.
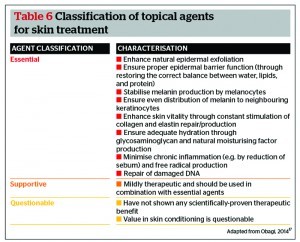
When selecting a skincare range to successfully treat rosacea, clinicians must be guided by science and results, not patient comfort. The author’s choice is ZO® Skin Health (Irvine, CA), which provides all of the active ingredients (both essential and supportive agents) necessary to effectively treat and maintain skin17. Tables 6 and 7 detail a list of these agents, and their associated characteristics. Questionable agents should be avoided entirely, as they have not shown any scientifically-proven therapeutic benefit. Of note, approximately 80% of currently available cosmeceuticals use active ingredients that fall under the questionable category17.
ZO® Skin Health contains two product lines; ZO® Medical and ZO® Skin Health. The ZO® Medical range is used when treating diseased states as it is more aggressive, while ZO® Skin Health is used for daily skin care, prevention, maintenance, and anti-ageing17. For the purpose of this article, the author will focus on ZO® Medical because the treatment of rosacea, a diseased state, is being discussed (Figures 2 and 3). The select procedures and oral medication further detailed remain the author’s first choice in clinical practice.
Topical agents
Epidermal correction
These three critical steps form the foundation of basic daily skin hygiene. An oily skin cleanser (Oilacleanse™) should be selected to remove sebum and other impurities contributing to inflammation. An exfoliating scrub (Vitascrub™) will lift dead keratinocytes, and enhance the natural exfoliation cycle. Replete with vitamins A, C, E and C-Esters, it will also assist in barrier function maintenance. To remove any residual sebum and minimise pore size, oil control pads (Cebatrol™) containing a blend of acids, alcohol and witch hazel should be used. Mandelic acid specifically targets the inflammatory cascade to reduce irritation, while triclosan delivers antibacterial benefit. An emollient complex is further added to soothe skin and reduce redness.
Disease-specific agents
This optional step has two possible subcategories as follows:
- Epidermal exfoliation (Glycogent™) — the addition of alpha hydroxy acid chemical exfoliants. This increases cell turnover to minimise trapped sebum and expressive lesions. Skin texture is also softened, a particularly favourable outcome when patulous follicles and phymous changes are present in rosacea. Such pore minimisation will have a direct impact on suppressing the superficial output by the sebaceous gland
- Oil control (Aknetrol™) — supplementing micronised benzoyl peroxide to remove and control sebum. This is a useful step for patients with particularly oily skin. The benzyl peroxide acts as an antimicrobial agent, but by incorporating the micronised technology, irritation is eliminated. A number of key additives, such as grape seed extract, further calm redness and reduce inflammation.
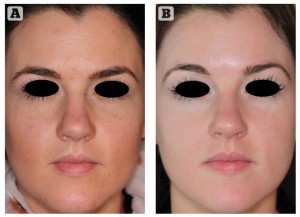
Figure 2 30-year-old female with rosacea treated for 18 weeks with ZO Medical (ZO® Skin Health, Irvine, CA) and oral isotretinoin (20 mg daily). (A) Before and (B) after treatment
Epidermal stabilisation
This step is paramount when treating both diseased and non-diseased skin. The serum (Daily Power Defense™) provides anti-inflammatory activity, antioxidant benefit, melanocyte stabilisation, DNA repair/protection, and renews barrier function. It also increases the skin‘s resistance to UV light, and the subsequent inflammation induced. Considering that sun exposure is a well‑documented rosacea trigger, this is acutely beneficial.
Vitamin A
The benefits of Vitamin A in treating and maintaining rosacea are countless3, 16, 17, 26. These include: barrier function restoration, epidermal thickening, increased tolerance, exfoliation regulation with more gelatinous stratum corneum, decrease in acneiform eruptions, evening of pigmentation, enhanced vasculogenesis, ageing suppression, improved moisturisation, pore size reduction, and collagen/elastin/NMF/GAG up-regulation. During the treatment phase of rosacea, retinoic acid should be used. For product and penetration enhancement, this is combined with Melamix™, and applied for three keratinocyte maturation cycles (18 weeks). After this period, the therapeutic properties of retinoic acid are exhausted, and chronic inflammation instead dominates. To avoid such irritation, retinoic acid should be replaced with a high dose retinol product (Radical Night Repair™ or Retamax™, both 1% retinol) after 18 weeks. This will maintain the results achieved, and circumvent unwanted product-generated inflammation. Bearing in mind that rosacea is a chronic condition, should it re-present during maintenance, the patient can resume use of the retinoic acid/Melamix™ temporarily. It is worth noting that Retamax™ also provides textural improvement through its retinol delivery mechanism. It is the first choice for maintenance among rosacea sufferers, and useful in collagen remodulation of phymatous states.
Pigmentation
Topical vitamin A (retinol or retinoic acid/Melamix™) will improve non-specific discolouration that typifies rosacea. Should a pigmentation disorder be present in conjunction with the disease, additional agents will be necessary. When rosacea coexists with conditions of pigmentation, the former drives the latter exponentially, making it more difficult to treat. For superficial pigmentation correction (e.g. ephelides), Brightenex™ can be used. Alternatively, Melamin™ (4% hydroquinone) is a more appropriate option when treating deeper disease (e.g. melasma). Specific to rosacea, both of these topicals contain antioxidants and immune response-modulating agents.
Sun protection
Sun exposure causes exacerbations of rosacea because of the inflammation it generates. To limit this, individuals should apply sunscreen suited to their condition. Interestingly, 88% of rosacea patients report a decrease in flares when they use sunscreen27. Previous sunblocks were thick and opaque, and exacerbated disease. Newer products contain micro-fine particles that are smooth and light, making them non-greasy and cosmetically acceptable28. A triple-defense system is advocated (Oclipse-C™ Broad Spectrum Sunscreen SPF 50), which protects through physical blocks, fractionated melanin, and antioxidants29. Rich in anti-irritation additives and barrier-enhancing agents, it is ideal for sensitive skin. Phytosphingosine further limits skin redness by inhibiting the pro-inflammatory cytokine, interleukin-1.
Controlling reactions
A number of products in the aforementioned regimen generate anticipated reactions (erythema, dryness, and exfoliation). These occur during the early stages of the programme, and diminish once the skin has built tolerance, and its repair ability has been strengthened. Anti-redness and anti-inflammatory nourishing agents (Ommerse™ Daily Renewal Crème, Ommerse™ Overnight Recovery Crème, or Restoracalm™) are provided to calm the skin during the reaction phase. Such topicals notably make use of Actimmune and plant stem cell extract technology to deliver phenylpropanoid glycosides, which have outstanding anti-inflammatory potential.
Sensitivity
On initial consultation, patients should be questioned about the presence of skin sensitivity. Among rosacea sufferers, this intolerance is usually because of irritation, and propelled by moisturiser misuse17. It is worth noting that true sensitivity does exist (xeroderma pigmentosum, atopic dermatitis), but this is separate and different. When sensitivity is present in the context of rosacea, a modified regimen should be started instead, focusing on barrier repair, dermal stabilisation, and inflammation reduction. This protocol will reverse moisturiser dependence and sensitivity in as little as 3 weeks. Products that induce anticipated reactions should only then be introduced.
Procedures
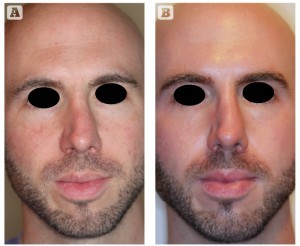
Figure 3 32-year-old male with rosacea treated for 18 weeks with ZO Medical (ZO® Skin Health, Irvine, CA) and oral isotretinoin (20 mg daily). (A) Before and (B) after treatment
There are two particular categories of lasers appropriate for rosacea. Resurfacing lasers improve the skin’s surface texture, including large pores, sebaceous gland hyperplasia, and rhinophyma30. The author’s preference here is a fractionated CO2 ablative laser. Vascular lasers (e.g. pulsed dye laser) are also useful when correcting persistent diffuse erythema and telangiectasia3.
Procedures should not be used in isolation, as they do not address the underlying pathophysiology. Furthermore, they promote sensitivity, disease and sebaceous gland activation. Rosacea must therefore be treated before the procedure, and steps should be in place afterwards to prevent any disease recurrence and unwanted side-effects.
Oral medication
As far back as 1981, the efficacy of isotretinoin in treating rosacea was observed31. Not only does it shrink the size of sebaceous glands and decrease sebum production leading to a reduction in papule and pustule counts, but oral isotretinoin also exhibits certain anti-inflammatory properties, rendering it effective in a variety of inflammatory dermatoses31, 32. Specific to rosacea, it has also been shown to reduce facial cutaneous blood flow, and nasal volume in rhinophyma. Particularly valuable is its ability to provide long-lasting disease remission after drug discontinuation31, 32.
New isotretinoin formulations with Lidose® technology are proving exciting. Isotretinoin is optimally absorbed in the presence of a fatty meal, but patients often forget when and how to take their medication. Formulations that already include the fat component in the pill matrix can help optimise drug absorption, even on an empty stomach2.
The author frequently treats rosacea using low levels of oral isotretinoin (20 mg per day). This dosage allows concomitant topical agent application, and it is better tolerated by patients. Treatment duration should last 3 months or more. Continuous microdose isotretinoin may be applicable in select cases to control flares, as long as appropriate precautions and monitoring are carried out.
The author does not advocate the use of antibiotic preparations (both oral and topical) in rosacea. Their ability to induce remission is poor in comparison to that of isotretinoin, and their use frequently becomes long term31. This creates ecologic mischief by altering immune systems and driving resistance17, 25. The limited benefits of antibiotics in rosacea are a result of their anti‑inflammatory properties, not an alteration of flora17, 31. However, should the clinician choose to introduce topical antibiotics such as metronidazole into the programme detailed above, it may be applied after Cebatrol™ in the disease-specific agent step, followed by the other ZO® Medical components. As a general rule, if skin fails to improve after two keratinocyte maturation cycles, any product should be discontinued.
Recent developments
Mirvaso® (brimonidine 0.33%; Galderma Laboratories, L.P., Lausanne, Switzerland) topical gel is a novel and exciting product, which launched earlier this year. An alpha‑adrenergic agonist, Mirvaso® stimulates alpha receptors in the smooth muscle layer of superficial skin vessels, resulting in vasoconstriction. It is the first product approved for the topical treatment of persistent (non‑transient) facial erythema2. Fortunately, Mirvaso® can be used long term without a decrease in efficacy. Studies have also shown improvement starting on the first day of application, and lasting up to 12 hours33. It is, however, important to remember that this agent only improves a symptom — the vascular response of rosacea. It may be supplemented under the disease-specific agent step, but Mirvaso® does not replace the other crucial agents, which comparatively treat the disease and halt its advancement.
Make-up
Clients with diseased skin will often seek advice on cosmetics for coverage. These can camouflage the embarrassing redness and lumpiness of rosacea, while medical therapy works to banish the underlying condition.
The key for rosacea patients is to select products that are allergy-tested and suited to sensitive skin. Mineral make-up is ideal, as it is not oil based and does not clog pores28. Equally important, pure minerals free from rosacea triggers such as artificial fragrance, dye, talc, peppermint, eucalyptus oil, menthol, and alcohol should be sourced. A patch test on a peripheral area may be useful before applying a product on the face, to determine whether it affects the individual’s skin.
Formulations that contain broad-spectrum sun protection are particularly appealing, as are those with silica to diminish the appearance of pores and a rough texture28. Some mineral powders are specifically developed to colour-correct redness. Innovative manufacturers even tailor-make products to complement rosacea treatment, with ingredients such as oat beta glucan that can reduce redness by up to 40%.
For both treatment and appearance reasons, medication should be applied before make-up. A recent study found that most patients had a good cosmetic appearance when make-up was applied over topical therapy, and this did not cause rosacea symptoms to worsen34. Equally important is regular cleansing of application brushes, which can harbour oil and bacteria.
Conclusions
The strawberry face that Dr AJ Cronin described, and the exaggerated rosacea illustrations used historically for diagnosis, represent an extreme state of the disease. In reality, the signs and symptoms are much more discrete, and require careful investigation by the clinician. Early and accurate diagnosis is vital, so that treatment remains proactive rather than reactive. A combination of topical agents, procedures, and oral medication is advocated by the author, who also estimates prevalence rates significantly higher than those previously recorded. The wild and patchy underdiagnosis of rosacea is alarming, when undoubtedly it is a vast condition; indeed, the strawberry fields of dermatology