Robotic surgery arose gradually to overcome human limit with technical developments. Until recently, the most common option for hair restoration involved follicular unit transplantation (FUT), whereby a strip of scalp is surgically excised and individual follicular units (hair grafts) are generated via bench-top manual dissection. Manual follicular unit extraction (FUE) using small dermal punches was first introduced in 2002 to avoid moderate pain and a linear scar after FUT. However, FUE procedures can be quite tedious and slow, also the surgeon needs to undergo special training, and, along with this, there’s a significant learning curve. With the aid of the ARTAS Robotic System, surgeons can harvest FUE grafts precisely and constantly with a low transection rate and at high speed.
Over the past decade, robotic procedures have advanced care in many surgical categories. Robotic systems have been proven to assist surgeons with difficult, repetitive and precise surgical movements, reducing manual variability, and improving outcomes. Their reproducible accuracy and precision has also enabled less invasive techniques that allow more patients to be treated and to have better experiences.
Robotic surgery arose gradually over the past two decades, advanced by technical developments and also driven by the desire to address some of the shortcomings of both open and laparoscopic surgery. The company that is most frequently credited with being the pioneer of robotic surgery is Intuitive Surgical®. In 1999, they introduced the da Vinci® Surgical System, which introduced robotic surgery to the public. Among the advantages of the da Vinci® System are superior 3D HD visualisation, enhanced dexterity, greater precision and control, as well as ergonomic comfort in minimally invasive surgery1. The da Vinci® System allows surgeons to perform even complex procedures, such as heart valve repair and cancer surgery, through 1–2 cm incisions.
The use of robots has expanded what is possible clinically and paved the way for future innovations. The advantages of minimally invasive surgery are very popular among surgeons and patients, owing to the reduced recovery and decreased pain.
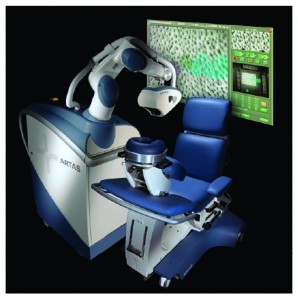
Restoration Robotics, Inc., was founded by a team of physicians and engineers with expertise in image-guidance and surgical robotics, and were inspired to develop a solution for hair transplantation. Robotic technology is used in a variety of surgical and diagnostic procedures and plays a unique role for follicular unit extraction (FUE)2. Uncertainty about the procedure, results, visible scarring, and the long recovery times are key obstacles for many patients interested in hair restoration. They are looking for a less invasive technique that provides consistent, safe results. Restoration Robotics introduced robotic technology to deliver safe, accurate and consistent results in hair restoration. No other company to date is involved in robotics in hair restoration. The ARTAS® Robotic System (Restoration Robotics, Inc., San Jose, CA) enables physicians to achieve reproducible, natural-looking outcomes with fast recovery times for patients (Figure 1).
Current state of hair transplantation
Until recently, the most common option for hair restoration involved follicular unit transplantation (FUT), whereby a strip of scalp is surgically excised and individual follicular units (hair grafts) are generated via bench-top manual dissection. This has been the common practice in FUT since the 1990s. A newer development, manual follicular unit extraction (FUE) uses small dermal punches to remove single hair grafts directly from donor sites and then implant them in the balding areas of the scalp3. This coincides with a trend in medicine towards less invasive procedures and reduced recovery times.
While FUE seems like an obvious minimally invasive option for patients, practitioners have been slow to adopt the procedure. For physicians to become proficient at FUE, they need to undergo special training and along with this, there’s a significant learning curve. Analysis of the angle, direction, and type of skin is a complex process requiring extensive experience. Until the surgeon has acquired this experience, the process can be quite tedious and slow. Although FUT is an efficient means of harvesting large quantities of follicles, patient recovery time and scarring are significant. Another drawback is that this is a surgically invasive procedure for the patient.
The ARTAS® Robotic System is FDA-cleared and has a CE mark. The first procedure performed was in October 2006. It is a physician controlled, interactive, computer-assisted system that enables harvesting of hair follicles during hair restoration procedures. It combines an image-guided robotic arm, special imaging technologies, small dissection punches, and a computer interface and is capable of identifying and harvesting individual follicular units to implement the FUE technique.
By using advanced digital imagery to map and analyse hair in its natural scalp groupings to extract the most viable and robust intact follicular units, the author has found the quality of grafts obtained to be superior to other methods. In the author’s experience, the ARTAS® Robotic System provides an excellent opportunity to improve patient care and outcomes. The physician is able to provide the patient precise, consistent and robust hair grafts for optimal results.
Benefits of robotic technology for FUE
The ARTAS® Robotic System is the first and only technology that allows physician-controlled, image-guided, robotic-assisted FUE. The theory behind applying robotic technology to FUE was that if you could actually remove all of the decisions regarding angles and directions required by the physician and use technology to determine those factors, you could take a physician with little experience and after a few hours of training, they could produce grafts with the ARTAS® Robotic System as well as a physician with many years of experience.
The image-guided robotic arm is programmed to be able to do with great precision what physicians can do only with extensive experience. Specialised cameras and digital mapping are able to automatically assess the angle and direction of each follicular unit. Sophisticated algorithms then determine the hair density, as well as the proper angle and depth of incision required to effectively harvest the units.
The robot can harvest follicular units in a random pattern, according to distance limitations, or as a percentage of the total number of follicular units in a designated area. The physician can make minor adjustments to dissection depths and angles during the extraction process, to ensure the patient receives optimal results. Although there is physician involvement, the robot is doing most of the repetitive actions; therefore, making the process much faster.
While in general, FUE is less invasive, it is a traditionally slow method for extracting hair follicles. An average physician performing FUE may only be able to extract 200 to 300 grafts in an hour4. With the robotic assisted system, they are able to extract 500 to 1000 grafts per hour5. Additionally, comparisons of traditional FUE to robotic assisted FUE also reveal the computer’s ability to produce better grafts. Newcomers to FUE often experience follicle transection rates of 20 to 30% when first learning the procedure. Preliminary studies conducted by the author’s team at Seoul National University Bundang Hospital in Korea have demonstrated a 4.9% transection rate on Korean patients. It is a very safe method for consistently extracting a high volume of healthy, intact hair grafts rapidly. Follicular units require little or no trimming and are ready to implant immediately after harvesting, which increases graft success rates and reduces technician time.
The process is simple. The robot quantifies the digital images it captures, each and every hair follicle’s image is captured 50 times a second. Every hair shaft is a vector and every vector has an angle, direction, and length. Clusters of vectors indicate that a follicular unit has more than one hair shaft. Vectors have thickness (hair calibre) and the robot is able to calculate the distance between vectors. It is programmed to know the location of each hair on the surface of the scalp and recognises and adapts to movements. The robot is enabled to make rapid decisions as it harvests the hair follicles.
The surgeon makes incisions in the scalp with needles or blades to create aesthetically natural recipient sites and patterns. The surgeon also decides where the hairline is located based on aesthetic judgement and incisions are made to match the hair angles and directions of the pre‑existing hair, while carefully avoiding any pre‑existing hair. The surgeon also determines density and distribution of recipient sites.
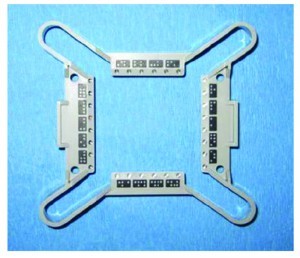
When a patient comes in, the author would cut his hair down to 1 mm in length. This allows the imaging system to identify and map each follicular unit. The patient is then anaesthetised and placed in the chair designed especially to be ergonomically comfortable for the patient. A 3.5 x 3.5 cm skin tensioner (Figure 2) is then placed on the patient’s scalp. This skin tensioner, which has fiducial markings as reference points, provides the mechanism by which the system tracks all of the follicular units, follows patient movement, and allows precise control of incision depth.
With the skin tensioner in place, we then begin harvesting. Red lights appear which heighten the contrast between the hair follicles and the skin, and the ARTAS® Robotic System then analyses them with the assistance of a set of cameras. The technology determines the location, angle, and direction of each individual hair follicle and is able to determine almost instantaneously the proper approach to harvest each follicular unit. The image- guided robotic arm begins harvesting the hair follicles in random patterns, according to the harvest spacing set by the physician. These random patterns make the procedure virtually undetectable after the wounds have healed.
A sharp bi-bevelled needle with an inner diameter of 1 mm first scores the skin, and then the follicular unit is dissected with the more blunt rotating outer punch. Light vacuum suction is used to assist in elevating the follicular units from the skin, and the physician is able to extract and evaluate them. Once harvesting is complete in one area, the skin tensioner is moved to the next area of the scalp.
Physician and patient experience
The author has found transitioning to the ARTAS® Robotic System to be a relatively straightforward process. Manual FUE is a tedious and imprecise process even for experienced physicians. After a few hours, owing to fatigue, transection rates tend to increase. The ability to use the ARTAS® technology to do so much of the minute calculations and precision punching offers numerous advantages.
Developers of the ARTAS® Robotic System installed a number of safeguards into the technology. The first of these is a built-in force sensor that constantly monitors the forces that are exerted by the tips of the punches. If the force goes above a certain threshold, the system backs away, prompting the physician to check before resuming treatment.
There are sensors around the casing of the mechanism itself, ensuring that if the casing touches the patient, the System automatically backs away from the patient. This prevents the patient from feeling as if they are being pushed. Another safety feature is the motion detector that is continually monitoring the patient. As the patient moves, it adapts or pauses until the physician can verify that the patient is ready to proceed. During the clinical trials of over 350 patients, no safety related adverse events occurred5.
In addition to the sensors, the needles have markings to indicate depth. Images are constantly being taken of the robotic dissection that can be viewed on the user interface. By using simple arrows the surgeon can then indicate if the needles need to incise deeper into the skin or more shallow.
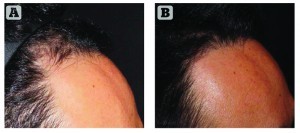
The author has found that patients can achieve a permanently robust and improved hairline, meeting their cosmetic goals in a very safe and effective manner (Figure 3). The image-guided robotic arm, under the control of a physician, has the ability to assist in making decisions about which grafts to extract and how to approach the grafts. This is able to expand physicians’ capability to provide quality results to their patients, which has been somewhat lacking with FUE.
This less invasive procedure is beneficial for patients as well. Healthy grafts with ample protective tissue can be transplanted efficiently. Patients incur no linear scar or stitches as with other hair restoration options, and experience faster healing and less downtime. They can return to normal activity in 3 days or less. Following strip-based surgery, the donor site will not heal for 7 to 10 days or until sutures are removed (Figure 4). Many strip-based surgery patients report a sense of tightness and some degree of numbness for 2 to 3 months after a strip harvest. There is also a higher incidence for prolonged discomfort.
Key patient benefits
- Robotically precise and consistent
- Reduced treatment times
- Decreased discomfort and anaesthesia
- Faster healing and recovery
- Avoids a linear scar
- Nearly undetectable donor area.
The future of hair restoration
Through recent improvements in software and hardware upgrades, transection rates with the ARTAS® Robotic System have dropped to around 5%. Productivity has also increased to being able to deliver 700–1000 grafts per hour, and the author is now able to do cases greater than 1500–2000 grafts. Even for physicians with minimal experience, after a few hours of training, they can produce grafts as viable as those achieved with many years of experience.
This less invasive method represents a new way to attract prospective patients who would not normally consider hair restoration surgery, owing to its traditional recovery time and visible scarring, among other factors. This new technology, which improves patients’ overall hair restoration experience has an important adjunct for a surgeon’s practice. The addition of the ARTAS® Robotic System may attract many patients who would otherwise be apprehensive about the traditional drawbacks associated with FUE. Patients who are satisfied refer other patients from other parts of your region, which can grow your practice.
The ARTAS Robotic System lets physicians take hair restoration technology to a new level, and transforms the hair restoration experience for patients. It eliminates the need for sutures or staples and delivers permanent, natural-looking results with minimal scarring, short recovery time, and high patient satisfaction. Following the ARTAS® Procedure, patients can confidently wear their hair in any style, long or short, without concern about hiding a linear scar from traditional strip surgery. Additionally, built-in safeguards help to preserve the natural look of the donor area.
The author can anticipate that robotics will lead the future of a number of medical fields outside of hair transplantation. This is a very exciting technology for practitioners who want to offer their patients the most advanced methods available.