Marina Neves Cavada, Oswaldo Luiz Fontoura Carpes, Aline Silveira Martha, Luise Sgarabotto Pezzin, Juliana Mazzaferro Krebs, and Denise Cantarelli Machado, demonstrate an innovative new technique to perform nasal tip refinement and avoid unnecessary complications
The nasal tip is a complex structure whose integrity is maintained by an interrelated network of supporting mechanisms made up of both the tip cartilages and the ligaments connecting them1. It is the most important determinant of a refined nose2. Tripod is an analogy used to better understand the nasal tip support. It is a dynamic unit that is suspended and supported by its rigid surrounding structure deriving from the nasal bones, pyriform aperture, and nasal septum1.
Before making any meaningful changes to the tip, it is necessary to stabilize the nasal base, which is composed of the caudal septum and its soft tissue attachments to the lower lateral cartilages. The major nose tip support mechanisms are the size and shape of the alar cartilages, the attachment of the medial crura to the septum, and the attachment between the cephalic edge of the lower lateral cartilages to the upper lateral cartilages1.
After aesthetic reduction rhinoplasty, a 25% decrease in cross-sectional area and 13% decrease in the piriform aperture at the nasal valve can be achieved3. Moreover, 50% of patients post-rhinoplasty have internal nasal valve reduction4.
The nasal tip structure is viewed as an integrated structure in which the disruption of one element affects the stability of the whole1. Creating a natural nasal tip contour is a complex task and requires a three-dimensional approach. Once a solid foundation has been created at the nasal base, the tip can be modified1.
Several studies have shown the potential of mesenchymal stem cells (MSCs) for tissue engineering and cell therapy. The MSCs can be obtained from several tissue types, each one carrying its own characteristics5,6. In this article, the authors present the mesenchymal potential of the osteocartilaginous paste graft discarded during rhinoplasty to fill in the nose tip. The results pointed to an ideal autologous source for a scaffold cartilage to maintain the ideal nose structure.
Anatomy
Nasal tip support was classified by Tardy in three major and six minor mechanisms1. The three major mechanisms are (1) the size, shape, thickness, and strength of the medial and lateral crura; (2) the attachment of the medial crura footplate to the caudal border of the quadrangular cartilage; and (3) the attachment of the caudal border of the upper lateral cartilage to the cephalic border of the low lateral cartilage. The minor tip-support mechanisms are thought to augment the major ones1.
The nasal septum supports the cantilever from its undersurface. Particularly at its caudal aspect, the quadrangular cartilage, functioning as a pillar, carries much of the burden of nasal tip support in most noses1.
The nasal valve is the narrowest cross-sectional area of the nasal cavity with the greatest resistance to airflow in the whole respiratory tract8,9. It is divided into external and internal portions. The columella, the nasal floor, and the caudal border of the lower lateral cartilage form the external valve. The internal nasal valve is located in the transition area between the skin and the respiratory epithelium and is composed of the septum, the caudal end of the upper lateral cartilage, and the anterior end of the inferior turbinate10.
Although tip analysis can be subjective, decisions must be made and an operative plan formulated. The goal of analysis is to determine what the tip characteristics are and how far they deviate from the ideal. The size, angle, shape, and type of nose varies between different races, ages, and sexes11. The knowledge and understanding of the variations in nasal structure between different ethnic groups is critical to the rhinoplasty surgeon as the goal is to achieve functional and aesthetically pleasing results2,12. Knowing the structural and soft-tissue differences helps to select effective surgical manoeuvers2.
Nasal tip support techniques
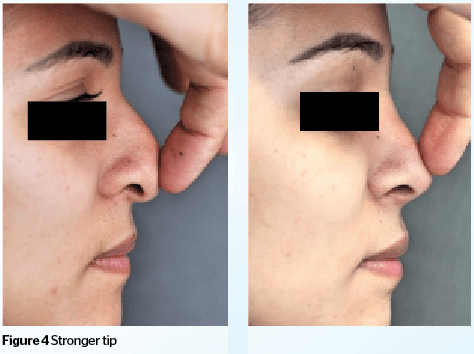
Tip surgery can seem extraordinarily complex due to the wide variation in tip anatomy, patient desires, and surgical options5. Tip position is a consequence of the combined forces of the three legs of the tripod as well as the support provided by the caudal septum. Proper stabilization of the base enables the surgeon to place the nasal tip in the desired position and avoids postoperative loss of tip projection1.

The combination of an open approach and tip suturing has revolutionized tip surgery, allowing the surgeon to control the individual tip characteristics of width, projection, definition, and supratip break. Suturing provides a graded controlled method of tip shaping.
The five components of the procedure were as follows:
- Create symmetrical rim strips
- Insert and fix a columellar strut
- Domal creation sutures for definition
- An interdomal suture for tip-width control
- A tip-positioning suture to create a supratip break.
Tip refinement grafts to the sutured tip can give the requisite shape and definition, which elevates and refines the final result5.
This article discloses a new rhinoplasty technique to be combined with the traditional surgical techniques used to refine and support the nasal tip. It displays great aesthetic results and protects the nasal valve.
Materials and methods
This article is a retrospective study that describes a new technique performed on 254 patients during 3 years (January 2013 to January 2016). The indications were nasal hump, weak framework, and slightly wide tip.
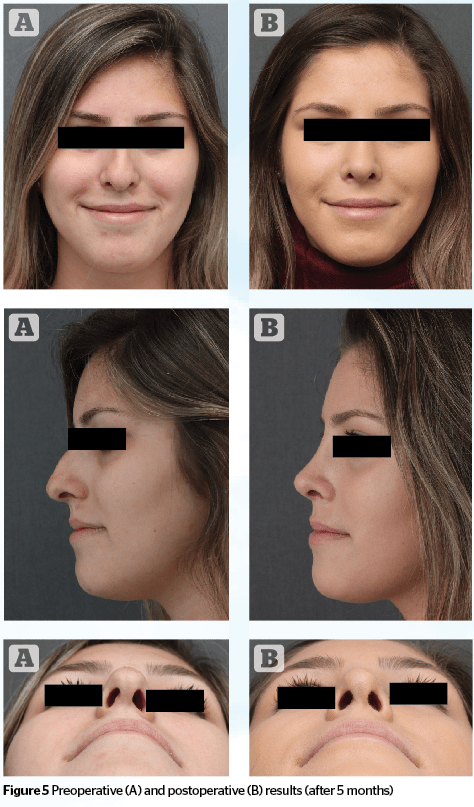
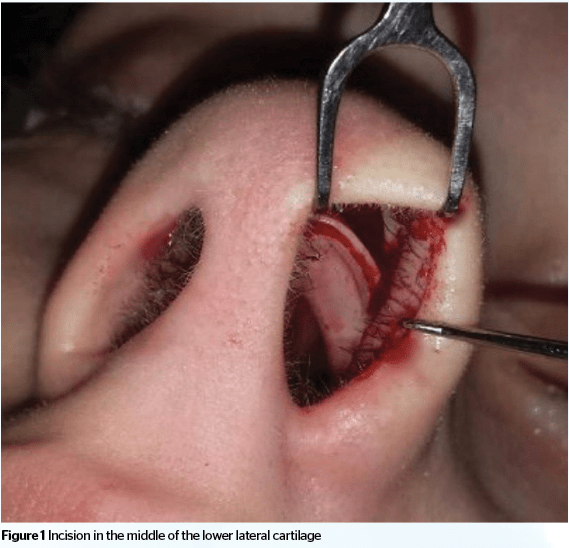
The newly proposed technique consists of the traditional treatment to the dorsum (Figure 1); a fine rasp is used to remove the excess dorsum and the tissue that is removed turns into a soft paste that can be molded into the desired shape (Figure 2). After making the necessary adjustments and changes to the nose, a small bilateral incision is made in the caudal edge of the lower lateral cartilage, where a narinary incision is traditionally made, but only in its top curvature (transition with medial crura). The purpose of this incision is to create a pocket for placing the paste, in order to shape the tip according to the surgeon’s desire (Figure 3).

The osteocartilaginous paste was plated on a six-well petri dish with Dulbecco’s Modified Eagle’s medium (DMEM; Gibco, Life Technologies, USA) supplemented with 10% fetal bovine serum (FBS; Invitrogen, Calif., USA), 100 U/mL penicillin, 100 U/mL streptomycin, 100 μg/mL gentamicin, and incubated at 37°C, under 5% CO2 with humidity. The media was changed twice to three times a week. After one week, the osteocartilaginous paste was discarded, the adherent cells were detached with trypsin/EDTA solution and transferred to a new plate. When cell confluence reached 70%, cells were subcultured.
Plastic adherence and morphology were confirmed by observation under inverse microscope (AxioVert 25, Zeiss). Osteogenic differentiation was induced by culturing the MSCs with DMEM supplemented with 0.5 μm dexamethasone, 108 mmol/L β-glycerol phosphate and 5 μg/mL ascorbic acid. After three weeks, matrix mineralization was detected by Alizarin Red Staining.
Results
The histological analysis of the osteocartilaginous paste graft showed small fragments of skeletal muscle and mature bone tissue.
MSCs were successfully obtained through culture from the osteocartilaginous paste and fulfilled the criteria to be considered MSCs after four weeks. Osteogenic differentiation was confirmed by specific staining.
After 6 months, biopsy was performed on noses of 3 patients
that underwent the technique described and the histological result confirmed the presence of hyaline cartilage.
Discussion
Frequently, a wide tip nose is treated using the traditional rhinoplasty technique, which consists of making a marginal incision, separating the lower lateral cartilages (LLC) from the skin, pulling down LLC and finally making sutures at the domus. This may result in a weak nose structure. According to Beatty at al, placement of a narinary incision produces a 25% loss in tip support in all vectors13.
The nasal valve region plays a key role in nasal breathing14 and accounts for up to 50% of the nasal resistance in the upper respiratory tract. All these structures are often resected or disjointed in rhinoplasty, and may cause weakness in the cartilaginous support15. Grymer states that there is a 25% decrease in the cross-sectional area at the nasal valve after aesthetic reduction rhinoplasty3. As the nasal valve is a delicate area, protecting its functionality is one of the aims of the technique described. The use of traditional techniques to treat a wide tip nose with a weak framework can produce nasal dysfunction and poor aesthetic results.
Although tip refinement grafts to the sutured tip can give the requisite shape and definition, which elevates and refines the final result5, in some cases it can lead to nasal valve dysfunction.

The correction of post-rhinoplasty nasal obstruction requires a detailed history and careful evaluation of the nasal valve area in order to exclude other causes of obstruction, such as deviated septum and rhinitis. A number of techniques have been improved over the past few years to treat post rhinoplasty nasal obstruction. Spreader grafts and alar-batten grafts are the most widely accepted methods with reliable long-term outcomes9. These grafts, made by septal, conchal or rib cartilage, reinforce the lateral nasal wall structure and prevent its collapse during inspiration. Even though these techniques are available, the gentle proper surgical technique with a good understanding of nasal physiology allows the surgeon to perform a concomitant aesthetic and functional approach without interfering with the nasal physiology10,16.
The new technique using an osteocartilaginous paste graft 
The narinary incision made to insert the paste can prevent the use of the intercartilaginous incision, traditionally used to treat the dorsum. This new technique prevents the disruption of the joint and ligaments between the upper and lower lateral cartilages that can lead to a postoperative collapse of the nasal tip, which can occur with the intercartilaginous incision.
Conclusion
Refining the nasal tip with an osteocartilaginous paste graft is a remarkable new technique that works as an outstanding alternative to traditional techniques. This surgical manoeuvre enables the refinement and support of the nasal tip. Furthermore, it prevents nasal valve insufficiency.