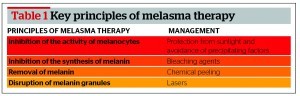
Melasma is a common acquired disorder of skin pigmentation. It occurs typically as symmetrical, irregular, light-grey to dark-brown macules and patches primarily in females with darker skin types, at puberty or later in life. It involves sun-exposed areas, such as the face and arms. Patients with epidermal type melasma show an excellent response to therapy, patients with mixed type show a good response, while patients with dermal melasma show a poor response to therapy. Key principles of therapy include the inhibition of the activity of melanocytes (protection from sunlight and avoidance of precipitating factors), the inhibition of the synthesis of melanin (using bleaching agents including phenolic compounds, non-phenolic compounds, and combination formulae), the removal of melanin (chemical peelings), and the disruption of melanin granules (lasers). Treatment should be individualised and tailored to each patient’s needs. An important challenge with melasma treatment is that it commonly relapses after treatment, thus necessitating maintenance therapy.
Skin colour is influenced by a variety of factors, such as melanin, capillary blood flow, and collagen in the dermis. For the most part, however, the colour of the skin is controlled by the pigmentary system and is primarily determined by the quantity, type and distribution of melanin within the skin. The synthesis of melanin is a complex multi-step process, catalysed by at least one or a number of enzymes, the most prominent of which is tyrosinase. Pigmentation disorders are broadly divided into hypermelanotic (excess melanin but normal melanocytic population) and hypermelanocytic (excess melanin and increased melanocytic proliferation), as well as hypomelanotic/amelanotic and hypomelanocytic/amelanocytic, which are caused by melanin deficiency and a reduction or absence of melanocyte numbers, respectively. Further categorisation distinguishes these groups into congenital and acquired, circumscribed, mixed and generalised, epidermal, dermal, and mixed1,2.
Melasma, a term derived from the Greek word melas, meaning black, is an acquired hyperpigmentation cutaneous disorder. It is a common acquired hypermelanosis that occurs exclusively on sun-exposed areas, mostly on the face and occasionally on the neck and arms, and it is more common in women (female to male ratio of 9:1) and in darker skin types3,4.
Pathogenesis and clinical presentation of melasma
The aetiology of melasma remains poorly understood but it is mostly attributable to sunlight and genetic predisposition.
The main risk factor is exposure to natural or artificial ultraviolet (UV) radiation5. Also, hormonal factors have been implicated in the pathogenesis of melasma, as it more commonly affects females, it is associated with hormonal disturbances or the intake of oral contraceptives and it can be aggravated during pregnancy6,7. An increased number of oestrogen receptors that stimulate melanocytes, resulting in their upregulation, has been demonstrated in melasma8,9. Also, cosmetics (oxidised linoleic acid, salicylate, citral, preservatives), phototoxic or photosensitive medication, and anti-convulsants have been associated with melasma10.
Lesions of melasma demonstrate excess melanin in the epidermis and dermis. Increased expression of alpha melanocyte-stimulating hormone (α-MSH) in keratinocytes and C-kit in melanocytes of lesional skin have been reported11–13. Histological examinations have shown that melasma lesions, in addition to increased pigmentation, have more elastosis and vascularisation than perilesional skin. No increase in the number of melanocytes was noted in those areas, but the melanocytes were larger, intensely stained cells with very prominent dendrites, and showed increased melanogenesis, especially producing eumelanin14.
The diagnosis of melasma is made clinically. It presents as irregular, light to dark brown, grey, blue or black macules and plaques, mainly on the face, and also on the neck, V-area of the chest, or rarely on the upper extremities. Mucosae are not affected10.
Depending on the location of melasma on the face, it is classified in three clinical types15:
- The centrofacial pattern. This is the most common pattern. It involves the forehead, cheeks, upper lip, nose, and chin (Figures 1 and 2)
- The malar pattern. This involves the cheeks and nose
- The mandibular pattern. This involves the ramus of the mandible.
Also, melasma is classified in four histological types based on the depth of the location of melanin as assessed by Wood’s lamp examination16:
- In epidermal melasma, the pigmentation is intensified under Wood’s lamp examination. It is the most common type of melasma. Melanin is increased in all epidermal layers
- In dermal type melasma, the pigmentation is not increased under Wood’s lamp examination. Many melanophages are found throughout the entire dermis
- In mixed type, there is increased melanin in the epidermis and many melaninophages (macrophages) in the dermis, while during Wood’s lamp examination there is intensification of melanin in some areas, while in others there is attenuation or no change
- In indeterminate type melasma, observed in Fitzpatrick skin types V–VI, there are no findings with Wood’s lamp examination.
Patients with epidermal type melasma show an excellent response to therapy, patients with mixed type show good response, while patients with dermal melasma show a poor respone to therapy10.