Frédéric Braccini, Anis Mrad, and Philippe Kestemont provide a literature review and delve into their personal experience of non-surgical rhinoplasty treatments

ENT and FPS, L’artistique Medical Healthcare Center, Nice, France; Anis Mrad, MD, ENT and FPS, Beirut Lebanon; Philippe Kestemont, MD and FPS, FPS , Nice France
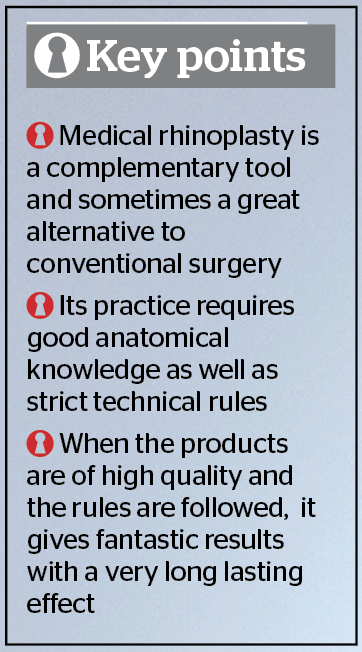
Rhinoplasty remains above all a highly surgical procedure but the emergence of fillers and botulinum toxin leads us to new approaches regarding indications and treatment.
We were one of the first teams in the international literature to report and publish the results of using fillers in the nose back in 20081–3. and also published the first book on this field of interest4.
In this article, and based on our experience of more than 1000 cases of medical rhinoplasty, we will provide an extended analysis of this procedure, its indications and the management of complications that may appear4,5.
The aims of the treatment require an artistic analysis of the nose: we must consider the nose ‘by itself’, the nose ‘in the face’, and in three-dimensions. We will modify:
- The nose in its unity and volumes, which correspond to nasal volumetry
- The nose in the face; for this we must consider the global harmony of the face (in particular the nasofrontal angle, nasolabial angle and cheekbone projection).
Contemporary treatment of the lip and chin with fillers is a means to achieve a real medical profiloplasty. The treatment of cheekbones, in particular, and their projection, allows us to influence the ‘relative volumetry of the nose’, especially on profile views.
Anatomical bases
Anatomical basis are essential to determine the location of the treatment and understand the potential risks related to the injections1,6-9.
The nose represents the middle third of the face. It is an empty triangular pyramid with an osteochondral structure, where the base is the nostrils and the top corresponds to the nasal root. Over this osteochondral frame lies a perichondrial and periosteal envelope, a muscular layer, and the skin.
Understanding the two elements of the nose (Figure 1 and 2):
- A fixed part, formed by the bridge of the nose, the rising part of the maxillae, the nasal bones, the upper lateral cartilages (triangular cartilages) and the nasal septum.
- A mobile part represented for most by the lower lateral cartilages (major and minor alar cartilages) with the lower part of the triangular cartilages, that play a major role in the nasal valve.
Analysing the relationship between the mobile and fixed elements is critical in the treatment plan before a medical or surgical rhinoplasty.
Practical applications arising from this relationship refer to the morpho-dynamic anatomy concept. Hyaluronic acid injections are performed deeply, in contact with the cartilage or bone structures.
That is to say, the knowledge of nasal structure in both soft tissue and the nasal frame is crucial before starting a medical rhinoplasty treatment with filler products.
There are various muscles related to the nose: elevators, depressors, nares compressors or dilatators. They play a modest role except for the tip depressor muscle that lowers the nasal tip and increases dorsum kyphosis. The naris dilator muscles can be active and enlarge the nasal base.
The elevator labii superioris alaeque nasi muscle extends the nose length, increases dorsum kyphosis and reduces the nano-labial angle, exposing the superior gum (gummy smile). This muscle, with the nasalis and procerus muscles in the median line, favour the appearance of ‘bunny lines’.
All these muscles can respond to a botulinum toxin procedure and shall be selectively disabled as each case may need.
The nose is highly vascularized with small blood vessels, except for the internal canthus region. This vascularisation depends on arterial branches of both internal and external carotid arteries — the ophthalmic and facial arteries, respectively. Veins drain mostly to the angular vein as well as the facial vein.
Despite this abundant vascularisation, there is little risks of hematoma, whereas the major risk consists of vascular embolisation, in particular in the nasal ala and glabella.
Tip injections are not harmful if the practitioner respects conventional technical precautions10,11.
Motor branches come from the facial nerve and sensitive branches from the trigeminal nerve through infra-orbital and external nasal nerves. Injury of a nerve branch during a procedure usually has no significant implication.
Injection products
We have used many filling products for these indications. It is important to inject products that will benefit from a perfect balance between homogeneity, diffusion potential in filled areas, and, most importantly, safety1.
The use of permanent fillers for these treatments is contraindicated2.
Over years of research and experience, the choice for our favoured material to use was hyaluronic acid because it is considered relatively safe to inject in all facial regions: in the fixed nose area and in the nasal tip area (where we care about the tolerance of the product due to high cutaneous tension). The product must be stable, characterised with full tolerance and safety1,10–12. The product must be composed of a highly reticulated hyaluronic acid for better stability and longevity2,3,10.
Injection techniques
Ideally, the intervention should be made after the application of an anaesthetic cream on the treated surface. However, it can also be done with no anaesthesia at all. The nasal tip is the most sensitive part. A detailed treatment plan should be established before commencing the injection. Indeed, the nasal cutaneous tension, in particular in the tip area, is so important that if too many injections are made, the product tends to extrude1,13,14.
Treatment procedures
Filling the hump/working on the dorsum area
Obliquely at 45°, introduce the needle until reaching the bone. Hold the injection needle with the dominant hand, while pressing on the sidewalls of the nasal bones with the thumb and the index of the other hand. This prevents any diffusion of the product laterally, which is undesirable, up to the level of the inner canthus and the lacrimal ducts. Sometimes, filling the nasofrontal angle via lateral access is necessary to get a satisfactory result. A thorough massage of the product should be performed at the end.
Obtaining a beneficial result in ‘longer noses’ is achieved by increasing the anterior projection of the frontal area, thus giving the impression visually that the nose is ‘shortened’.
Avoid large boluses; small boluses are always recommended and always aspirate before injecting the filler. The reference technique is to use a 25 G cannula.
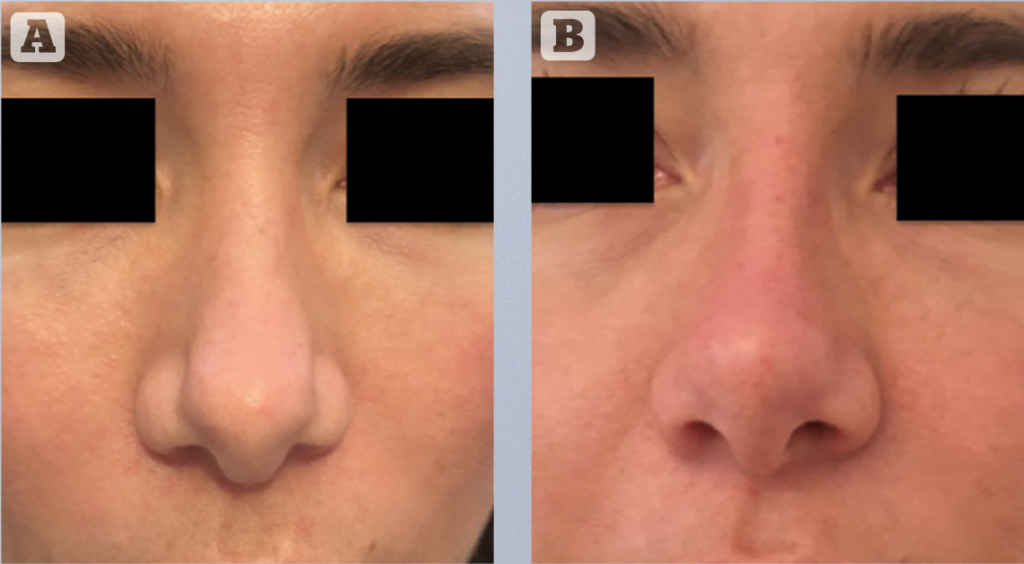
The tip definition
Indications for tip correction can be lifting in case of ‘parrot beak-shaped’ noses (drooping tip) or to give more definition and contour as in cases of a box nose shape.
As underlined earlier, we have to avoid multiple injection points. Injection pressure is essential — the procedure as to be slow and progressive to avoid cutaneous strain. The tip shouldn’t whiten under the effect of the filling. In our experience of over 1000 nasal injection procedures, we have never observed cutaneous necrosis. In order to avoid any cutaneous injury, the injection has to be slow and progressive2,10.
The face and nose, in particular, are very richly vascularized and there are numerous substitution networks. For a cutaneous necrosis to appear, these networks have to be ‘overwhelmed’. Embolisation risks are therefore more important with low reticulation products (long possible migration to the distal capillaries). This is one of the reasons why we recommend the injection of a high concentration and high reticulation product in the nasal area1.
Treatment of the columellar region and opening of the nasolabial angle
This can be achieved when there is no plan to inject botulinum toxin at the same time. The injection of the product has to be deep in contact with the nasal spine to open the angle. After that, the columellar lines can be balanced more superficially1.
This procedure can also be performed with a 25G micro-cannula.
Treatment protocol
After a full discussion with the patient about the desired and expected results, the application of HA injections to correct the nasal deformities, and clarification of potential complications, a consent form should be signed. An overcorrection should be avoided during the first procedure, and a follow up to be scheduled two weeks later. If necessary, a second injection is performed to achieve satisfactory results; these can remain stable for 18-24 months1,2,12–15.
Ultrasonography before and after injecting nasal fillers
The reflected sound waves, picked up by the probe and directed to the processor, are transformed into digital images. When a Doppler system is integrated with ultrasound, it is a called a duplex. With a duplex machine, blood flow is made visible on the screen in red and blue colours. Blood vessels can be identified along with the other dermal structures. All HA fillers bind to water and are thus hydrophilic. As water content does not reflect the sound waves, hyaluronic acid appears black (echogenic) or light grey (hypoechoic) on ultrasound (Figure 3 and 4)10,16.

Under ultrasonography guidance, the blood vessels can be easily visualised, and the tip of the cannula can be identified, thereby reducing the risk of intravascular infusion of the filler.
With ultrasound/duplex examination, skin and the underlying tissue, including muscles, veins, and arteries can be made visible. At the same time, any filler can be brought into sight, measured in pocket size, and the plane of injection can be viewed10, 17,18.
Moreover, the use of 2-dimensional laser speckle flowgraphy (LSFG) can identify ischemic states. It is used to evaluate skin blood flow after the injections, which can help predict the development of skin necrosis11,19.
Ultrasound can be a great aid for the treatment of adverse events after HA injections. It is well known that dissolving the filler will eliminate many of the adverse events. As mentioned above, hyaluronic acid fillers are easily detected with ultrasound. The pocket-size and the location of the filler can be brought into sight. Under ultrasound guidance, hyaluronidase can be injected directly into the filler pocket responsible for the adverse event10,20.
Indications of medical rhinoplasty
Not all rhinoplasties can be realised medically. Medical rhinoplasty is a wonderful alternative solution but also a complementary tool of conventional surgery. These two options of treatment should not be opposed. The surgeon has to know the benefits and limits of each. The indications are formed through the assessment and treatment plan, just as for a surgical rhinoplasty. A computerised morphing can be created before the treatment.
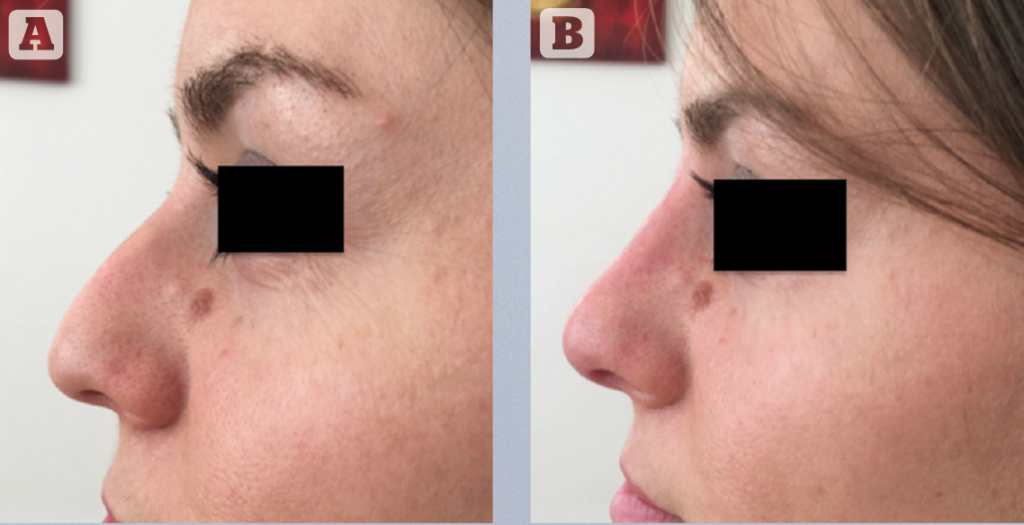
Augmentation rhinoplasty with reduction of the osteocartilaginous kyphosis
This is the best indication for medical rhinoplasty. Indeed, the nasal tip treatment and the filling of the junction along with lip and forehead injections gives remarkable results1.
After surgical rhinoplasty
All irregularities (depression of nasal bridge, asymmetry, deviation) can be filled by fillers. The indications for these treatments are the same as those for cartilaginous grafts. The injection of a filler following surgical rhinoplasty can be very interesting too. In some cases, adherences are revealed after the removal of the nasal splint (mobilisation of a bone or a cartilaginous fragment). In this case, it is very useful to ‘remove’ this adherence with a bolus of hyaluronic acid to avoid a permanent retraction. Fibrosis appears in the filled space after multiples injections, and in many cases, this manoeuvre can avoid a surgical procedure1.
The possibility of post-rhinoplasty correction represents an important safety advantage and considerably reduces the possibility of dramatically bad results. This improves the satisfaction of the patients, as alternatively, no surgical revision is recommended for at least 1 year after surgery.

Aesthetic and functional approach of rhinoplasty
The use of hyaluronic acid in the septal-triangular valve region is a way to counter the area’s collapse occurring after surgical rhinoplasty. This technique is very interesting because of its simplicity. Following a xylocaine naphazoline local anaesthesia, a direct trans mucosal injection is performed. The quantity of product to be injected is generally between 0.1 and 0.3 CC either side. This injection replaces the surgical use of spreader grafts and has to be repeated once or twice a year to stabilise the result. This treatment carried out in conjunction with an aesthetic procedure at the same time1,2.

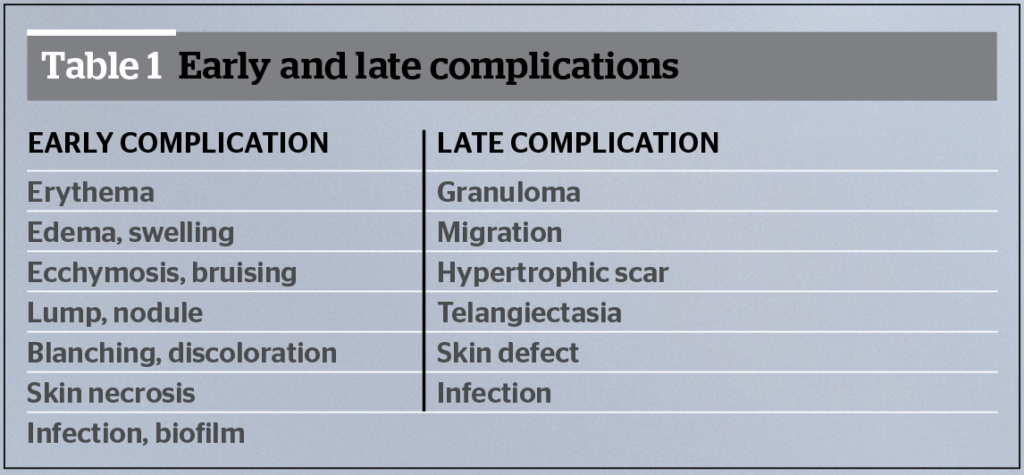
Complications of medical rhinoplasty with fillers
These can be related to the injection site. The literature reports minor complications, such as ecchymosis, granulomas, oedema and allergic reactions10–11. Management of such complications is the same as for the rest of the face.
Two major complications have been reported: skin necrosis and vision loss.
Skin necrosis can result from local ischemia when injections are too superficial (localised necrosis), or from distal embolisation (extensive necrosis). These local ischemic events can be found in cases of tip injection, nasal dorsum injection, and glabella injection12. Embolic necrosis events can be related to glabella and nasolabial fold injections13. Skin ischemia with necrosis usually evolves positively with moderate scarring and does not contraindicate further injection procedures. Initial symptoms can be a simultaneous local blanching, followed by blue discolouration of the skin, then necrosis. The patients suffer from immediate and abnormal pain at the injection site. Infectious complications can occur and have been described after hyaluronic acid injection14.
Embolic complications that relate to vision loss are usually related to hyaluronic acid injections and lipofilling located in the glabella or nasolabial fold15. Retrograde embolisation is the main accepted theory, in terms of physiopathology, for why such complications occur. Direct injection in the dorsal nasal artery or the supratrochlear artery results in occlusion of the ophthalmic artery. Angiographic findings after visual loss following dermal facial filler injections are specifically related to retinal ischemia: diffuse with distal occlusion when injecting hyaluronic acid or proximal occlusion with retrograde ischemia with lipofilling. Initial clinical signs are sharp abnormal retro-bulbar pain with immediate visual loss and sometimes ophthalmoplegia16. There is little to no management consensus for these complications.
Dayan et al.18 have suggested the use of hyaluronidase in all cases of vascular compromise, independent of the filler type, because of its oedema-reducing benefits and theoretical advantage in reducing the occluding vessel pressure.
Skin necrosis needs to be treated with local injection of hyaluronidase every 6 hours, Lovenox 0.4mL, systemic steroids (1 mg/kg/day for 3 days), utilisation of nitroglycerine paste, and wound healing with hyperbaric oxygen therapy. Although aspirin and intravenous (IV) prostaglandins have been suggested, their efficacy has not been proven19.
Antibiotics and antiviral may be required in addition to local superinfections.
In cases of sight loss the recommendation is to inject during the first 90 mins, the hyaluronidase through a retrobulbar injection with an acute 27 G needle in the inferolateral part of the orbital arch, along the floor of the orbit1,20. The aim for treatment is dissolving the product, facilitating blood flow, and promoting vasodilation.
Conclusion
Injectable rhinoplasty has high efficacy and can achieve very beautiful and stable results. An artistic approach is important to realise this technique and to adapt the treatment. This technique requires good anatomical knowledge, the use of suitable products and to follow strict rules in order to avoid side-effects dominated by embolic migration of the injected product.
Declaration of interest None
Figures 1-5 © Dr Braccini
Tables 1 © Dr Braccini
REFERENCES
- BRACCINI F et all. Medical rhinoplasty concept. State of the art. Rev laryngol otol rhinol 2017;138,2:53-56
- BRACCINI F. New trends in rhinoplasty. Rev laryngol Otol Rhinol. 2011; 132,4:215-221
- BRACCINI F, DOHAN EHRENFEST DM. Advantages of combined therapies in cosmetic medicine for face ageing: Botulinum toxin filler and mesotherapy. REV LARYNGOL OTOL RHINOL (BORD). 2010;131(2):89-95
- REDAELLI A, BRACCINI F. Medical Rhinoplasty. Basic principles and clinical practice. Ed. OEO Firenze 2010
- BRACCINI F, DOHAN EHRENFEST DM. Medical rhinoplasty: Rationale for atraumatic nasal modelling using botulinum toxin and fillers. REV LARYNGOL OTOL RHINOL (BORD). 2008;129(4-5):233-8
- BRACCINI F, PORTA P, THOMASSIN JM. Mini-rhinoplasty. REV LARYNGOL OTOL RHINOL (BORD). 2006;127,1:15-20.
- BRACCINI F, BERROS P, BELHAOUARI L. Botulinum toxin, description and clinical applications in the treatment of the face wrinkles. REV LARYNGOL OTOL RHINOL (BORD). 2006;127(1-2): 105-11
- REDAELLI A. Medical rhinoplasty with hyaluronic acid and botulinum toxin A: A very simple and quite effective technique. JOURNAL OF COSMETIC DERMATOLOGY. 2008;7:210-220
- BRACCINI F. In: Anatomy and volumizing injections. The nose. Fillers and rhinoplasty. E2e Medical publishing. Master Collection 2. 2013:105-122
- FUNT D, PAVICIC T. Dermal fillers in aesthetics: An overview of adverse events and treatment approaches. CLIN COSMET INVESTIG DERMATOL. 2013 Dec 12;6:295-316
- DE BOULLE K, HEYDENRYCH I. Patient factors influencing dermal filler complications: Prevention, assessment, and treatment. CLIN COSMET INVESTIG DERMATOL. 2015 Apr;15,8:205-14
- HONART JF, DURON JB, MAZOUZ DORVAL S, RAUSKY J, REVOL M. A case of nasal tip necrosis after hyaluronic acid injection. ANN CHIR PLAST ESTHET. 2013 Dec;58(6):676-9
- CHEN Q, LIU Y, FAN D. Serious Vascular Complications after Nonsurgical Rhinoplasty: A Case Report. PLAST RECONSTR SURG GLOB OPEN. 2016 APR 21;4(4):E683
- CHADER H, BOSC R, HERSANT B, LANGE F, HERMEZIU O, et al. Infectious cellulitis of the face complicating injection for esthetic nasolabial sulcus by hyaluronic acid: Report of seven cases. ANN CHIR PLAST ESTHET. 2013 Dec; 58(6):680-3
- CARRUTHERS JD, FAGIEN S, ROHRICH RJ, WEINKLE S, CARRUTHERS A. Blindness caused by cosmetic filler injection: A review of cause and therapy. PLAST RECONSTR SURG. 2014 Dec; 134(6):1197-201
- Kim YK, Jung C, WooSJ, Park KH. Cerebral angiographic findings of cosmetic facial filler-related ophthalmic and retinal. J KOREAN MED SCI. 2015 Dec;30(12):1847-55
- JOO K et all.Treatment Algorithm of Complications after Filler Injection: Based on Wound Healing Process Journal ok Korean Medical science, Nov 2014, 29 (Suppl 3):S176-S182
- Dayan SH, Arkins JP, Mathison CC. Management of impending necrosis associated with soft tissue filler injections. J Drugs Dermatol 2011; 10: 1007-12
- Kim SG, Kim YJ, Lee SI, Lee CJ. Salvage of nasal skin in a case of venous compromise after hyaluronic acid filler injection using prostaglandin E. Dermatol Surg 2011; 37: 1817-9
- DeLorenzi C. New High Dose Pulsed Hyaluronidase Protocol for Hyaluronic Acid Filler Vascular Adverse Events. Aesthet Surg J. 2017 Jul 1;37(7):814-825





