Catharina Shab, Manuela Lisandru, and Arna Shab describe a new treatment option for vaginal rejuvenation
email: [email protected]
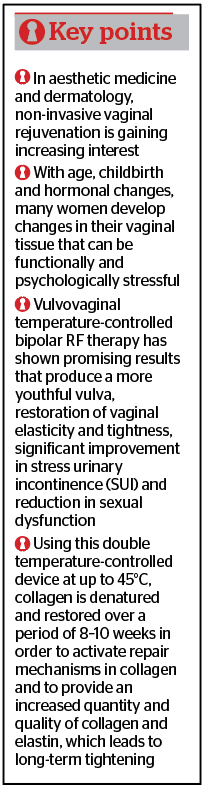
The female genital area is a complex entity. Many changes take place in the course of a woman’s life. Between birth and menopause, the vagina and nearby tissues are subject to numerous changes that lead to a well-defined range of conditions, including atrophic vaginitis, stress urinary incontinence (SUI), and various manifestations of sexual dysfunction and orgasmic difficulties. Treating this tissue region is problematic because women traditionally have difficulty discussing these issues with doctors. In addition, in some parts of the world there is a social bias towards women who are open about these issues. Therefore, until recently, resignation to these conditions was common and problem-solving was limited.
For a long time aesthetic medicine seems to have been focused on treating the face. However, women are increasingly focusing on the desire for rejuvenation in the genital area as well. Increased rejuvenation of the genital area is particularly noticeable through the application of non-operative energetic methods to the vaginal tissue in the same way as in aesthetic medicine1. Thermal effects cause neocollagenesis, increased blood flow, and coagulation or ablation, which activates healing factors. The release of thermal energy leads to a selective effect in the vaginal tissue. Targeted thermal energy on the vaginal wall can be used to treat the patient at higher energies with almost no pain.
Gyné RF
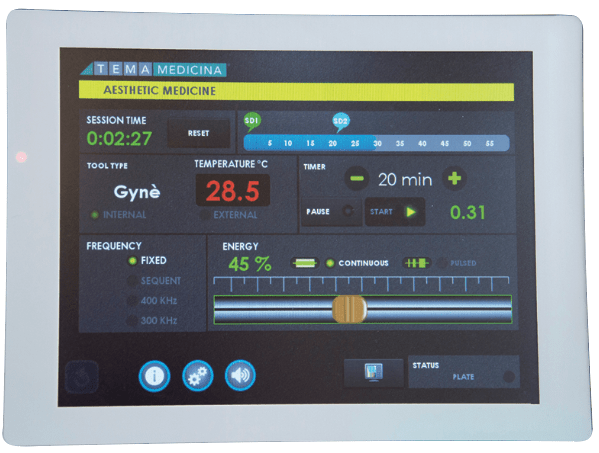
Gyné RF (ATTIVA®) is a device for performing transcutaneous temperature-controlled high-frequency therapy (TTCRF) in the vulvovaginal area. High-frequency technology (RF) has been successfully used in aesthetic medicine together with lasers to rejuvenate or tighten the skin on the face, neck, chest and other parts of the body2. Recent studies have shown that it is also useful for use in the vulva and vagina1, 3, 4.
RF is safe, non-invasive and effective — especially when used on naturally well-hydrated tissue. When the RF electrode conducts electricity through the skin, resistance generates heat that causes the therapeutic damage required for rejuvenation: denaturation and contraction of collagen, activation of fibroblasts, increased blood flow and neocollagenesis2. Gyné uses a slim treatment probe specially developed for this task and adapted to the vaginal shape1.
The body of the handpiece appears in a tubular form with a tip that is cut at 45 degrees and rounded. It has two modes of treatment: internal surface, thus endovaginal, and external for the external genitalia. With the endovaginal treatment, the body of the handpiece has its surface covered by ceramic coated, coiled electrodes that cover the whole perimeter of the cylinder. Such electrodes function in a capacitive bipolar mode, with the utmost structural respect for the tissue. In between the electrodes, there is the internal thermal sensor, which is meant to continuously report the temperature on the screen and proceeds according to its changes, safely adjusting to the ongoing treatment.
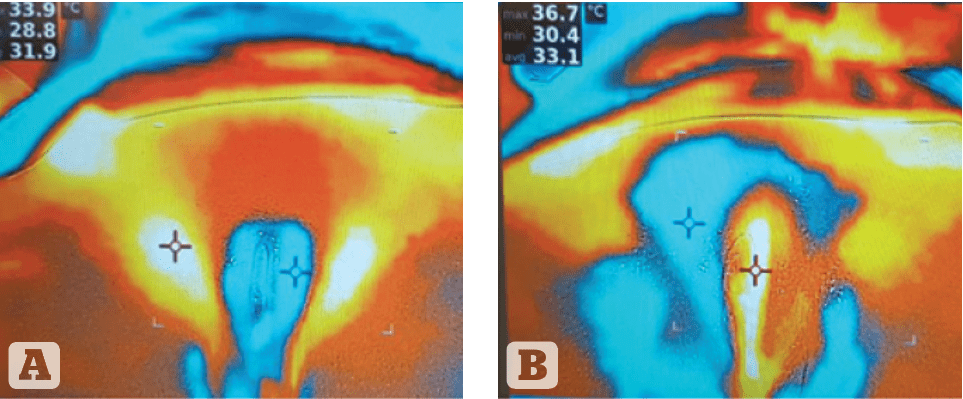
The feedback mechanisms on the probe include thermistors and thermocouples that provide the device itself with information on tissue temperature. This modulates the power output in such a way that scientifically defined temperature targets (42–45° C) are reached safely and quickly, but not exceeded, which prevents overtreatment (Figure 1).
Anatomy of the vulvovaginal area
The vulva is the outer part of the female reproductive system. It protects a woman’s sexual organs, urinary opening, vestibule, and vagina and is the centre of much of a woman’s sexual response. The labia majora are bilateral folds of skin with underlying fat and appendages running from the mons pubis and merge in the perineum. The labia minora are found just medial to the labia majora. The vestibule surrounds the opening of the vagina, or introitus, and the opening of the urethra, or urethral meatus. The vagina is a passageway beginning at the vaginal opening and ending inside the body at the cervix, the lowermost part of the uterus. The vagina is composed of a unique tissue that can expand and contract. The inner folds of the vulva form a hood of skin called the prepuce or the hood of the clitoris. The clitoris is a sensitive piece of tissue that swells with blood when stimulated5,6.

The vagina is a fibromuscular tube, the walls of which are normally in apposition in the relaxed state; it is H-shaped in its central portion, the side walls being suspended by their attachment to the paravaginal lateral connective tissue from which they receive their blood supply. It is lined by a stratified squamous epithelium arranged into rugal folds, giving the epithelium accordion-like distensibility without laceration. A dense, thin layer of elastic fibres is found immediately beneath the epithelium. Beneath this is a well-developed fibromuscular layer. The fibrous capsule external to this muscular coat is rich in elastic fibres and large venous plexuses. There are no glands in the vaginal lamina propria and vaginal lubrication is provided by transudate from the blood vessels as well as by secretions of the Bartholin’s and Skene’s gland. The vagina receives its blood supply from the vaginal arteries and their anastomoses with branches of the uterine, inferior vesical and internal pudendal arteries5–7.
The ‘ageing vagina’
Ageing and obstetric perineal trauma can be the cause of trophicity and dimensional problems, such as dyspareunia and vaginal laxity, and lead to postpartum sexual dysfunction. This common condition can have a negative impact on a woman’s quality of life and sexual intercourse (Pauls et al. 2012).
Data suggested that ageing, pelvic trauma, and surgery evoke tissue denervation and devascularisation, anatomic alterations, and increased degradation of collagen; all of these may lead to a decrease in mechanical strength and predispose an individual to prolapse. It has been demonstrated that there is a reduction in protein content and estrogens in uterosacral ligaments, in the vagina, and in the parametrium of women with prolapse8.
Physiologic changes in a woman’s life, such as childbirth, weight fluctuations, and hormonal changes due to ageing and menopause, may alter the laxity of the vaginal canal, damage the pelvic floor, and devitalise the mucosal tone of the vaginal wall. These events often lead to the development of genitourinary conditions such as stress urinary incontinence, vaginal atrophy, dryness, and physiologic distress affecting a woman’s quality of life, self-confidence, and sexuality8–10.
Due to the lack of estrogen during menopause, vulvar skin usually becomes thinner and drier. Additionally, the labia minora may flatten or shrink, and the vaginal opening appears smaller. Vaginal tissue may also become thin and dry, making intercourse uncomfortable or painful.
Vaginal health is an essential component of active and healthy ageing in women at midlife and beyond11.
GYNÈ RF: vaginal radiofrequency
Physical basics
The structural feature of GYNÈ RF was designed not only with regard to its undeniable effectiveness, but also and especially with regard to the well-being of the patient during treatment. The shape and body of the handpiece appear in a tubular shape with a tip that is cut 45 degrees and rounded (Figure 2).
There are two treatment methods: inner surface, hence endovaginal, and outer for the external genitalia. During the endovaginal treatment, the surface of the handpiece body is covered by ceramic-coated, wound electrodes that cover the entire circumference of the cylinder. Such electrodes operate in a capacitive bipolar mode. Between the electrodes is the internal heat sensor, which continuously displays the temperature on the screen and proceeds according to the temperature readings and adapts to the ongoing treatment in complete safety. In flat mode, the flat and rounded tip contains two additional ceramic electrodes and the heat sensor for treating the external genitals, whether in the area of the mucous membrane or the skin. In this case, in addition to the numerical value of the temperature, there is also the option of performing the treatment with the thermal imager (Figure 1).
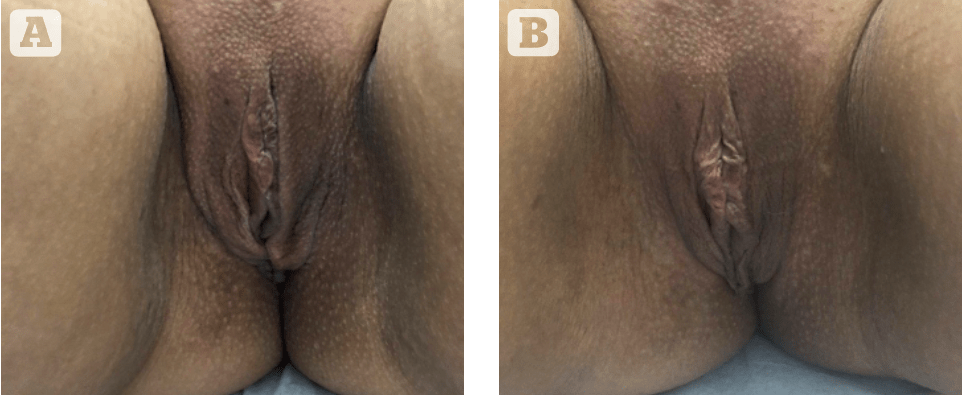
The patient’s well-being is ensured by the fact that, once the working programme has been selected, the handpiece that has been placed inside the vagina only needs turning 90 degrees per set time-cycle, with no need for further movements that might annoy or embarrass the patient. When it comes to the external mode, the coil is disabled while the electrodes housed in the rounded tip are activated, so that the operator is able to make the handpiece slide into the area to be treated, as the thermal sensor and the thermal camera support the work to be carried out. The treatment is comfortable and safe, and the perceivable results can be achieved from the first sessions. Moreover, before each session, the handpiece is covered in gel and coated with a sterile and disposable probe cover, so that the patient’s safety and the well-being are guaranteed. Treated patients present with restoration to the structure of the urogenital mucosa, leading to an improvement in the patient’s quality of life. From the first days following treatment, one may witness a reduction in burning, irritation, and dyspareunia, with a high degree of satisfaction. The possibility of using Attiva is extremely useful for managing vaginal and sexual female health, representing a therapeutic option also in those situations in which health professionals cannot intervene with traditional available therapies.
Conclusion
RF treatments for skin tightening are common, as they heat the dermis and subcutaneous tissues, thereby stimulating dermal collagen remodelling. It is well documented that dermal heating induces an immediate change in collagen structure followed by long-term stimulation of neocollagenesis12. These thermal effects can improve wrinkle appearance, skin laxity and contour of both face and body13–15.
Gyné RF is a safe, low-risk, easily applicable therapy option for practitioners and provides a particularly good alternative method for endovaginal and extravaginal tightening. Especially since downtime is not to be expected when using Gyné RF, this method can be expected to become the gold standard for this indication. The treatment with Gyné RF demonstrates through clinical studies and analysis a high degree of safety and efficiency. The treatment is characterised by its high tolerability. Thus, a realistic satisfaction of patient expectations can be achieved, with an excellent visible effect and a very grateful group of patients.
Declaration of interest None
Figures 1-4 © Dr Shab
References
- Alinsod RM. Temperature controlled radiofrequency for vulvovaginal laxity. PRIME. 2015;3(4):16–21.
- Key DJ. Integration of thermal imaging with subsurface radiofrequency thermistor heating for the purpose of skin tightening and contour improvement: a retrospective review of clinical efficacy. J Drugs Dermatol. 2014;13(12):1485–9.
- Millheiser LS, Pauls RN, Herbst SJ et al. Radiofrequency treatment of vaginal laxity after vaginal delivery: nonsurgical vaginal tightening. J Sex Med. 2010;7(9):3088–95.
- Sekiguchi Y, Utsugisawa Y, Azekosi Y, et al. Laxity of the vaginal introitus after childbirth: nonsurgical outpatient procedure for vaginal tissue restoration and improved sexual satisfaction using low-energy radiofrequency thermal therapy. J Womens Health (Larchmt). 2013;22(9):775–81.
- Hoare BS, Khan YS. Anatomy, Abdomen and Pelvis, Female Internal Genitals. SourceStatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020. 2020 Feb 27.
- Nguyen J, Duong H. Anatomy, Abdomen and Pelvis, Female External Genitalia. SourceStatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020. 2019 Oct 10.
- Hunter JG. Labia Minora, Labia Majora, and Clitoral Hood Alteration: Experience-Based Recommendations. Aesthet Surg J. 2016 Jan;36(1):71-9. doi: 10.1093/asj/sjv092. Epub 2015 Oct 24.
- Nappi RE, Martini E, Cucinella L, Martella S, Tiranini L, Inzoli A, Brambilla E, Bosoni D, Cassani C, Gardella B. Addressing Vulvovaginal Atrophy (VVA)/Genitourinary Syndrome of Menopause (GSM) for Healthy Aging in Women. Front Endocrinol (Lausanne). 2019; 10: 561. Published online 2019 Aug 21. doi: 10.3389/fendo.2019.00561
- Herzog AR, Fultz NH. Prevalence and incidence of urinary incontinence in community-dwelling populations. J Am Geriatr Soc. 1990;38:273-281.
- Palmer MH, German PS, Ouslander JG. Risk factors for urinary incontinence one year after nursing home admission. Res Nurs Health. 1991;14:405-412.
- Berek JS, Hacker NF. Practical Gynecologic Oncology. 2nd ed. Baltimore, Md: Williams & Wilkins; 1994.
- Sadick NS, Sato M, Palmisano D, Frank I, Cohen H, Harth Y. In vivo animal histology and clinical evaluation of multisource fractional radiofrequency skin resurfacing (FSR) applicator. Journal of Cosmetic and Laser Therapy. 2011;13:204-209
- Treatment of Skin Laxity Using Multisource, Phase- Controlled Radiofrequency Yohei Tanaka Additional information is available at the end of the chapter http://dx.doi.org/10.5772/intechopen.71749.
- Shab A, Lisandru M, Shab C. Subdermal Induced Heat (S.I.H.) Technology – a new option for skin tightening and fat reduction of double chin. Aesthetic Medicine, Volume 5, No4, October – December 2019, S. 11-15.
- Shab A, Lisandru M, Shab C. Skin tightening and fat reduction of double chin using Subdermal Induced Heat (S.I.H.) Technology – Case report. Kosmetische Medizin 1.20; S. 20-23






