Full title: A study to investigate the effectiveness of combining technology, prescription diet, lifestyle changes and biometric monitoring to achieve optimum weight loss and body image.
Obesity is a problem of epidemic proportions and despite public health measures, is actually getting worse. Being overweight or obese has significant implications on health and wellbeing and treating complications costs the UK National Health Service (NHS) hugely with regard to resources. Although there is evidence for dietary interventions and exercise, this study investigates an holistic approach combining diet, exercise, motivational support and non‑surgical body treatments, and its impact on body weight and other measurements. At the end of a 4-month period, 10 patients lost an average weight of 12.9 kg and 15.2 cm to the waist, as well as seeing improvements in blood pressure, cholesterol and mental wellbeing. Further research is planned to examine continuing the programme beyond 4 months, and also looking at a maintenance programme to maintain weight-loss.
England, along with the rest of the UK, has an unenviable position as one of the world leaders in excess weight. It has one of the highest rates of obesity in Europe and one of the highest in the developed world1. In England, most people are overweight or obese. This includes 61.3% of adults and 30% of children aged between 2 and 15 years1. People who are overweight have a higher risk of developing type 2 diabetes, heart disease and certain cancers. Excess weight can also make it more difficult for people to find and keep work, and it can affect self-esteem and mental health. Health problems associated with being overweight or obese cost the National Health Service (NHS) more than £5 billion (€6.1 billion) every year2.
Despite this, there is little help available on the NHS. A meta-analysis looking at the long-term efficacy of anti‑obesity drugs showed less than a 5 kg weight-loss over a period of 1–4 years3. It is for this reason that people are increasingly turning to the private sector. Weight-loss is a thriving industry, with over £1 billion spent on diet products in the UK alone last year4. Similarly, global equipment sales for body contouring devices have seen a rapid increase. Technology is more advanced and treatments are now more effective, more affordable, more available, and with less downtime for the average consumer.
However, devices do have their limitations and this study aims to determine the benefit of an holistic approach combining medical technology (3D-lipo device with cryolipolysis, cavitation, radiofrequency and vacuum rolling; 3D-Lipo Ltd., London, UK) with a lifestyle programme incorporating diet, exercise and wellbeing.
Study participants
Patients were recruited on a voluntary basis, after completing a medical history questionnaire and assessment. Exclusions to participation included pregnancy and lactation, patients under the age of 18 years, pacemaker or metal implants, eating disorders, immunosuppression, milk intolerance, and uncontrolled medical conditions.
A total of 10 patients were recruited with an average age of 37.7 years (range 25–45 years) and an average starting body mass index (BMI) of 35.8 (range 30.2–44.1), which is in the severely obese category. Nine patients completed the 4-month trial with one patient withdrawing from the study at 3 months owing to a change in life circumstances and depression. After the 4‑month period, patients were asked whether they would like to continue for a further 2-month extension period, of which five patients remained on the study. There were no financial incentives for participation and no cost to the patient.
Study protocol
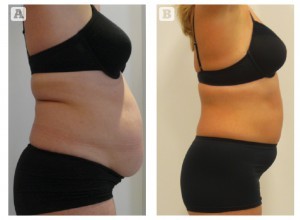
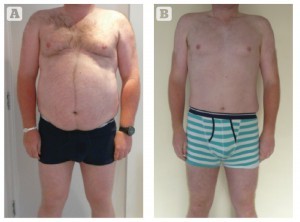
All patients were given an overview of the study and the time commitment involved. A consent form and confidentiality agreement were signed by each patient. At the initial consultation, biometric measurements were taken (Tanita Segmental Body Composition Scales; Tanita Europe BV, Amsterdam)5, health and wellbeing scores (The Warwick–Edinburgh Mental Well-being Scale), urine testing, blood testing (full blood count, renal function, liver function, thyroid function, glycated haemoglobin, cholesterol and high-density lipoprotein), blood pressure, and hip, waist and chest measurements. Standardised photographs were taken at the start of the trial and at 4-weekly intervals, and also on completion of the study.
Dietary advice was given throughout the programme and patients were provided with recipes, snacks and meal suggestions. Each patient had an allowance of protein, greens, starchy carbohydrates and a dressing calculated using a unique point-based system developed specifically for the study. The points were determined based on the patient’s basal metabolic rate (BMR) as calculated using the Tanita Body Composition Scales. The BMR gives a prediction of how much energy the body requires while at complete rest. This figure is then multiplied according to the amount of energy that is required to sustain a healthy lifestyle. The result was then converted into a simple points system that was individual for the patient, comprising a number for the snack component of their diet (ranging from 1 to 6) and a number for their main meal (ranging from 4 to 10). In this way, the authors ensured that the patient would not only get the correct balance of nutrients and vitamins in their diet, but also the right amount of energy in a way that would help balance blood sugar balance for the body.
The principles of the diet component consisted of a milkshake at 7 am, a snack at 10 am, a soup sachet at 1 pm, a milkshake at 4 pm, and a meal at 7 pm. If required as part of the programme, a further snack was allowed at 10 pm. The soups and milkshakes were provided to the patients and contained a special formulation that was specifically developed for the study, to encourage weight-loss and provide essential vitamins and nutrients. The formulation was derived after looking at various products on the market, which are already well established and have evidence for their use as part of a weight-loss programme, although they were additionally fortified with L-carnitine, which is known to support the metabolism of fat during weight-loss diets6.
The essence of the diet was to maintain a healthy, balanced blood glucose level throughout the day without any peaks or troughs. By doing this, patients did not feel hungry or have cravings throughout the day, and did not complain of lack of energy or feeling low. Although specific timings were recommended, there was flexibility to suit different lifestyles, although it was advised to try and have something to eat or drink every 3 hours. During vacation periods when patients were not preparing their own food, they were encouraged to continue on the soups and milkshakes and given additional advice on foods to try and avoid. After the initial 2 weeks, patients were allowed to have a cheat meal once per week, where there were no restrictions.
Exercise was agreed using the FITT principle (frequency, intensity, time and type) and concentrated on different domains (aerobic exercise, resistance training, functionality, and mobility and flexibility). Physical activity was measured and assessed using the Borg scale, which subjectively gauges the perceived exertion with each exercise. The Borg scale ranges from 6 (no exertion at all) to 20 (maximum exertion). Exercise was further discussed and encouraged as patients remained on the study. As participants were successfully losing weight, they found that they had more energy and were more capable of doing exercise. Exercise was tailored to the individual using a specific workbook and ranged from exercises as simple as getting out of a chair without using the arms to assist, to intense gym sessions with a personal trainer.
Treatments occurred on a weekly basis using the 3D-lipo device and comprised a combination of cryolipolysis, cavitation, radiofrequency and vacuum rolling. Although cryolipolysis was used at the start of the trial, the majority of treatments comprised cavitation (using the 3D-lipo machine, auto-programme setting was used, abdomen and flanks, P3 cavitation working mode, and a default 90 W power). Treatment was applied in individual zones for 10 minutes in each zone and a total treatment time with cavitation of 40 minutes). Vacuum rolling was used at the end of each treatment session. Each treatment lasted approximately 45 minutes and the area to be treated and the technology used was at the discretion of the clinician on an individual basis. For the duration of the programme, the average number of treatments received by each patient was 17.1.
Each patient had a unique treatment plan based on their own targets, their BMR and exercise capabilities.
Weekly visits
The patients attended on a weekly basis for a 3D-lipo treatment. Biometric measurements (including weight and BMR) and urine testing were carried out at each visit. During the treatment, further motivational, dietary and exercise advice was given, as well as further reinforcement of the programme. If targets were not being met, the patient was given the option to see the clinician to re-assess before the monthly visit. If any medical problems were identified, they were referred back to the clinician for further assessment and suitability to remain on the programme. During the course of the study, no-one was excluded on medical grounds.
Monthly visits
Patients were seen by the clinician on a monthly basis to review targets and adjust diet according to the points system. Blood pressure was recorded at each visit and photographs taken. Medical assessments were conducted and any concerns discussed. Exercise and diet was reviewed and further targets set.
During the 4 months, all patients received active treatment with an initial 2-week detox at the start of the programme. The detox phase included all elements of the programme, but with additional restrictions on diet and drinks; this included no alcohol, no carbonated drinks, avoiding tea and coffee, and no cheat nights.
It is well known that even successful weight-loss strategies do not seem to be very effective in the long term, and a systematic review found that only 15% of patients had a successful outcome over time (median 5 years)7. It is intended that when patients have completed their treatment and achieved their target weight, they will be given the option to enter a maintenance phase. This will include monthly visits with the clinician as outlined above, adherence to the diet programme and exercise regimen, but without any additional body treatments.
Results
Weight loss
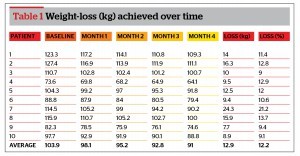
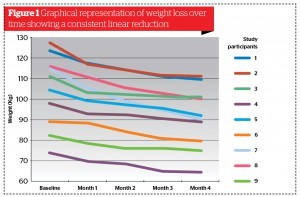
The average weight-loss achieved during the study was 12.9 kg (range 7.7–24.3 kg). However, as individual weights were so different at the start of the programme, weight‑loss is best described as a percentage of weight‑loss from baseline. The average percentage weight loss was 12.2% (range 9–21.2%). The average BMI at the start of the study was 35.8 (range 30.2–44.1) and 31.2 (range 26.5–38.7) at 4 months.
Body measurements
Hip, waist and chest measurements also showed significant improvement with an average reduction in hip size of 12.5 cm (range 6.5–22.5 cm), waist size of 15.2 cm (range 7.5–26.5 cm) and chest size of 7.3 cm (range 1–13.5 cm). All measurements were taken using a specific body measuring tape measure, and by the same person to ensure consistency. Self-reported improvement in body image was high.
Blood pressure
An average improvement in systolic blood pressure of 13.4 mmHg (range -2–34 mmHg) and diastolic blood pressure of 7.8 mmHg (range -2–27 mmHg) was observed during the study period. Blood pressure was recorded by the clinician using a standard aneroid sphygmomanometer. At the start of the study, one patient was known to be hypertensive and taking medication with an initial blood pressure of 129/86 mmHg and final blood pressure of 115/82 mmHg.
Blood tests
Full blood count, renal function, liver function and thyroid function remained stable throughout the study period. The average total cholesterol at the start of the study was 5.7 mmol/L and had improved by an average of 1.1 mmol/L on completion of the 4-month study. There was very little change observed in glycated haemoglobin levels with the HbA1c falling by 0.1%.
Urine tests
Urine dipstick testing was conducted on a weekly basis with the aim to detect ketosis. During the study period, there was only a single episode of a ketone-positive dipstick recording and this was during a viral illness and vomiting that the patient has been experiencing at the time.
Wellbeing self-assessment
Patients completed a WEMWBS (The Warwick–Edinburgh Mental Well-being Scale) to measure mental wellbeing at the start and end of the study8. The WEMWBS is a well-recognised peer-reviewed tool that was commissioned in 2006 to assess the positive mental health of the population, covering both hedonic and eudaimonic perspectives. All but one patient showed improvements in their scores, and an average improvement of 15.6% (range -2.9–37.1%) was recorded. The majority of patients had scores of between 40 and 59 at the outset, which lies in the average range and by completion, most patients were in the above average mental wellbeing range.
Conclusions
All patients who completed the study showed significant weight loss and improvements in body measurements, with favourable outcomes in blood pressure and cholesterol measurements. No adverse events were reported throughout the study and only one patient withdrew from the trial (although this was not felt to be related to participation in the programme). Feedback was very positive and this has been reflected in improvements in mental wellbeing scores.
Discussion
The results from this small study prove promising and by offering a combination approach using technology, diet, exercise and motivational support, seem greater than any of the individual components. In fact, a review of the literature looking at the evidence of non-surgical treatment states: ‘They do not serve as a significant method for weight loss, and as such, realistic expectations should be set with patients’9.
It will be interesting to see whether further weight-loss is obtained by continuing the study for a further 2 months, and the study has been extended to five patients who wished to continue on the programme and had not yet achieved their target weight. After completing 6 months, patients will also be given the option to remain on a maintenance programme involving continuing diet, exercise and motivational support and a monthly review assessment. Hopefully this will demonstrate sustained weight loss.
Finally, this has only been a small study including 10 patients, and it is hoped that when the programme is rolled out nationally, much more robust data will be available to confirm the findings of this trial.