The transcutaneous or subcutaneous administration of carbon dioxide (CO2) for therapeutic purposes is known as CO2 therapy or carboxytherapy. The effects of transcutaneous and subcutaneous administration of CO2 are active arteriolar vasodilatation, neoangiogenesis, artificial Bohr effect, and lipolytic effects. The use of CO2 is related to its positive and documented effects on different aspects of the imperfection’s aetiology. The adipose tissue is a connective tissue composed of fat cells, stromal elements, vessels (e.g. blood and lymph vessels), and a matrix of collagen fibres. Localised adiposity refers to the accumulation of fat in certain areas of the body. The goal of the therapy is to obtain a reduction in the volume of adipose masses, and therefore the use of CO2 is indicated either in combination with surgical treatment, or alone, if patients refuse surgical treatment.
Carbon dioxide (CO2) therapy refers to the transcutaneous or subcutaneaous administration of CO2 for therapeutic purposes. This treatment was developed in 1932 in the thermal station of Royat Spas of Clermont-Ferrand, France, which specialised in carbon gas balneotherapy in the treatment of patients affected by obliterating arteriopathies 1,2.
Italian contribution has been remarkable in this field of research; in 1964, Re et al published a monograph entitled ‘La cura termale delle malattie cuore e dei vasi‘ (Thermal therapy in the treatment of cardiovascular disease), which illustrated the importance of CO2 applications in these pathologies3.
In 1995, Parassoni, speaking at the XVI National Congress of Aesthetic Medicine in Rome, introduced the term ‘carbossiterapia’4 (carboxytherapy). Re and Parassoni also developed the first device for the administration of CO2.
Why CO2 therapy?
CO2 is one of the basic elements in the biological processes of plants and animals. It derives from the combustion of organic compounds in the presence of sufficient oxygen to complete the oxidation process. It is a colourless, odourless, inert, inflammable, and inactive gas, which is only toxic in elevated concentrations.
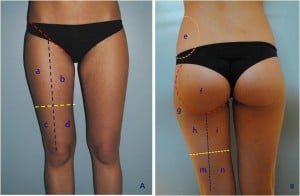
Figure 1 It is important to identify some landmarks in order to analyse the areas to treat. (left) Anterior view: red line = inguinal ligament; blue line = line from mid-inguinal ligament to knee; yellow line = anterior mid-thigh line. Area a = superoexternal thigh; area b = superointernal thigh; area c = inferoexternal thigh (external knee area); area d = inferointernal thigh (internal knee area).
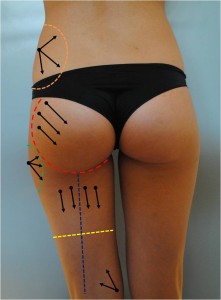
(right) Posterior view: red line = contour of buttock; orange line = contour of hip; green line = contour of trochanter; blue line = line from buttock fold to popliteal; yellow line = posterior mid-thigh line. Area e = hip adipocity area; area f = buttock area (muscle area); area g = trochanter adipocity area; area h = external superior thigh; area i = internal superior thigh; area m = inferior external thigh (external popliteal area); area n = inferointernal thigh (interior popliteal area)
At 0 °C, CO2 has a density of 1527 g/cm3 and its mass is 1977 kg/m3 in normal pressure and temperature conditions. It liquefies at a critical pressure of 73 825 bar and at the critical temperature of 31.06 °C.
Savin et al 5 in 1995, and Hartmann et al 6,7 in 1997, carried out experimental studies to verify the modifications induced by CO2 treatment on both microcirculation and the skin. They demonstrated the beneficial effects of transcutaneous CO2 administration on microcirculation in patients suffering from peripheral arteriopathies.
Furthermore, Brandi et al demonstrated the pharmacological properties of CO2 in plastic surgery and aesthetic medicine. As histological data showed the favourable effects of CO2 on collagenous fibre networks and major vascular and nervous structures, it became justified to use this technique in the treatment of localised fat and ‘fat-linked’ skin irregularities 8, or as an ancillary procedure following superficial liposuction 9. In 2010, Lee 10 confirmed Brandi’s results in a cohort of 101 patients with the same characteristics undergoing CO2 treatment. Possible applications of CO2 therapy in lipomatosis 11, chronic wound treatment 12, and vascular acrosyndromes 13,14 were also described.
Summarising, the effects of transcutaneous and subcutaneous administration of CO2 are:
-
Active arteriolar vasodilatation
-
Neoangiogenesis
-
Artificial Bohr effect
-
Lipolytic and lipoclasic effect.
-
These properties can be applied to the treatment of:
-
Peripheral arteriopathies and vascular acrosyndromes
-
Local adiposities and skin irregularities
-
Improving aesthetic outcomes after liposuction
-
Chronic wounds.