Drs Muhammad Humayun Mohmand, Muhammad Ahmad, and Armeela Javaid demonstrate an innovative way to avoid injecting filler material into blood vessels
Surgical facial rejuvenation is gradually being
replaced with non-surgical modalities, especially fillers (artificial or autologous). The popularity of non-surgical procedures is increasing day-by-day1. They are, however, associated with certain potential complications, ranging from minimal bruising on one end of the scale to blindness on the other2,3. There are multiple guidelines to be observed while injecting any filler to avoid intra-vascular complications. These include slow injection, blunt needles/cannulas, and regular withdrawal of the plunger before injecting.
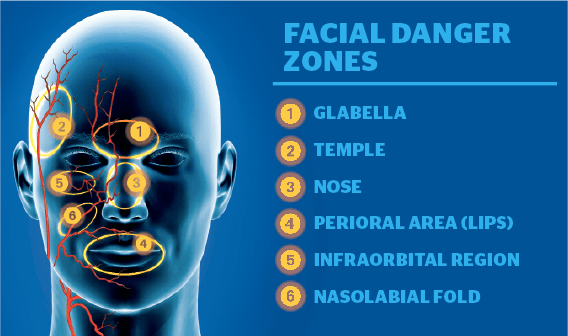
The face is one of the most highly vascularized areas of the body, supplied by vessels from both the external and carotid arteries. There are rich anastomoses among the vessels of both the systems. The literature mentions ‘six’ distinct places deemed as ‘facial danger zones’ where the anastomoses are found4,5. These ‘danger zones’ pose a higher risk of potentially devastating adverse events.
These include the:
- Glabella area (supraorbital and supratrochlear arteries)
- Nasal area (angular artery)
- Nasolabial groove (facial artery)
- Tear trough (infraorbital artery)
- Temples (superficial temporal artery)
- Lips/commissures (labial arteries)4,5.
Anatomical considerations
An extensive knowledge of anatomical variations is essential while undertaking filler injections to the face, especially around these ‘danger zones.’
Method

The needle depth is maintained depending on the anatomical considerations. Moreover, in the aging face, the course of the blood vessel may vary in different positions, i.e., in sitting or an inclined position, and it is important to make the markings in the inclined position in which the injections are to be administered.
Discussion
Human hearing can detect frequencies ranging from 20 Hz to 20 KHz. Ultrasound operates at frequencies higher (20 KHz) than this audible range6. Systems typically used in medicine have ranges far exceeding this, usually in the 1 to 20 MHz range. In the most basic state, ultrasound systems use short pulses of high-frequency sound emitted into the body. A combination of reflection, absorption, and scattering of the sound waves by varying tissues takes place and is recorded by the sensor. The frequency of the reflected sound waves can be used to determine the direction of blood flow through the Doppler effect6.
The use of Doppler ultrasound is not new in plastic surgery, it has been used previously to monitor flap circulation7,8. The frequency of ultrasound Doppler starts from 2 MHz to 10 MHz6. The handheld Doppler device sends and detects the reflected ultrasound, especially the moving erythrocytes. The use of probes and frequencies vary depending on the depth and diameter of the vessel, and there are a range of probes that can be used. The commonly used frequencies are 8 MHz and 10 MHz. The
use of gel improves the ultrasound conduction, while pressure applied by the probe on the vessel to be identified can also help. The direction of blood flow (toward the probe and away from the probe affects the loudness of the pulsating sound). The probe facing against the blood flow will detect the vessel with relative ease9. The sound intensity (loudness) returning from more resistance (blood flow coming towards the probe) will be louder than the sound intensity from the low resistance (blood flow away from the probe). Increase in the frequency of the probe decreases the distance of detection. For a probe with 8 MHz, the distance is 20 mm; whereas, with a 10 MHz probe, the distance is 12 mm10.
The use of handheld Doppler in the identification of the vessels is an important adjunct. Due to the wide variations in the distribution of blood vessels and their branching patterns, the extra care has to be undertaken while injecting the filler in the face, especially in the ‘danger zones,’ and specifically the area around the orbit. Use of a superficial veins visualiser (AccuVein®, AccuVein Inc. Huntington, NY, USA) can also help to mark out superficial veins.
Conclusion
The current technique gives an opportunity to mark the vessels to avoid serious complications of intravascular injections.





